NSQHS: Standard 6: COMMUNICATING FOR SAFETY BULLETIN MARCH | 2024
-
Introducing the Communicating for Safety 'Fab 5'
The ‘Fab 5’ is a team of multi-disciplinary leads brought together to support ongoing National Safety & Quality Health Service (NSQHS) Standard compliance.
The Fab 5 Team for NSQHS Std 6 is:
- Team Lead: Douglas Mill, DONM
- Quality Lead: Maree Dell, Best Care Coordinator
- Discipline Leads: Douglas Mill (Nursing), Rick Horton (Medical), Chris Weiers (Allied Health)
- Education Lead: Christine Pirotta
- Subject Matter Experts: Leanne Nuske (ADONM), David Smallwood (Deputy CMO), Lindsay Vernon (Mental Health)
- David Smallwood: Deputy Chief Medical Office
-
Do you have any questions?
For any queries about Communicating for Safety you’d like to direct to the NSQHS Std 6 Fab 5 or others, please contact BestCare@wh.org.au
-
Like to know more about Accreditation Readiness?
Visit our Live Best Care site at https://westerly.wh.org.au/livebestcare/ or use the following QR Code to find out more about NSQHS Standard Readiness.

From Doug
 As part of BAU Accreditation Readiness activity, a NSQHS Standard of the Month program has been introduced. This involves a focus on one Standard per month, with communications and walkarounds to help staff be aware of how Best Care at Western Health reflects this Standard, to ask staff possible Surveyor questions and answers, and to walk in a Surveyor’s shoes to see what WH practice looks like.
As part of BAU Accreditation Readiness activity, a NSQHS Standard of the Month program has been introduced. This involves a focus on one Standard per month, with communications and walkarounds to help staff be aware of how Best Care at Western Health reflects this Standard, to ask staff possible Surveyor questions and answers, and to walk in a Surveyor’s shoes to see what WH practice looks like.
We are excited that NSQHS Standard 6: Communicating for Safety is to be the focus of the first Standard of the month. This will run from Monday 4 March to Friday 29 March. Look out for friendly Best Care Co-ordinators, Fab 5 team members, and other staff who will visit clinical areas/departments to discuss Communicating for Safety with you.
During the month, we will also have a specific focus on the use of Communication Boards and staff engagement in the new Clinical Handover training module.
The Communicating for Safety Standard aims to ensure there is effective communication between patients, carers and families, multi-disciplinary teams and clinicians, and across the health service organisation, to support continuous, co-ordinated and safe care for patients.
The good news is we are already providing Best Care and living up to the requirements of this Standard in our everyday work! It is why we performed so well in the December 2023 Accreditation Survey.
Please continue reading to find out more about our Communicating for Safety strategies, achievements and opportunities for improvement, as well as resources to help you to continue to be Accreditation Ready for NSQHS Standard 6.
Douglas Mill
NSQHS Std 6 ‘Fab 5’ Team Lead
Director of Nursing & Midwifery
Our approach to Communicating for Safety
The NSQHS Standard 6 – Communicating for Safety is aimed at improving communication within healthcare organisations and reducing the risk of harm to patients.
Western Health’s comprehensive approach to Communicating for Safety draws upon the requirements of this Standard and supports the monitoring, review and improvement of safe care. Programs and strategies to help support communicating for safety include:
- Communication learning packages to support staff knowledge and use of effective communication techniques.
- Reviewing clinical incidents to look for themes around clinical communication and identify areas for improvement.
- Clinical handover protocols to support good communication between our healthcare teams and clear documentation of patient information.
- The use of an electronic medical record to help ensure patient information is easily accessible and up-to-date, which can improve communication between the healthcare team.
- Key roles and responsibilities related to patient identification processes across clinical and clerical workflows.
Resource Centre
The following resources have been put together to support staff to be aware of the NSQHS Comprehensive Care standard and Accreditation Ready for Survey against this Standard:
The following resources have been put together to support staff to be aware of the NSQHS Comprehensive Care standard and Accreditation Ready for Survey against this Standard:
- NSQHS Standard 6 Accreditation Walkaround Questions and Answers
- NSQHS Standards at a Glance
- Health Standards (NSQHS) WeLearn Module
Patient Story

Using ISBAR
After an unexpected death in one of our chronic care services, the family were obviously distressed. Being a very spiritual family the operations manager used the ISBAR process to communicate the need for urgent pastoral care.
The pastoral care manager was able to quickly understand the situation and what was required and had pastoral care support on site with the family within 30 mins.
The family were very grateful for the support in this difficult time.
Using the information provided, the manager recognised that other patients may have been traumatised in the unit and facilitated a pastoral care visit for each of the other 20 patients.
Without the use of ISBAR the urgency of this situation would have been delayed. There is no doubt that it allows fast and accurate transfer of information to ensure our patients and carers receive best care.
Improvement Initiatives
There are multiple improvement initiatives underway to improve Communicating for Safety. Do you know about these?
- WeLearn package to set the standard for Clinical Handover has been rewritten to make it contemporary and applicable to all craft groups
- Reviewing clinical incidents to see look for themes around clinical communication to identify areas for improvement continues at every meeting of the committee
- Replacement of the electronic program to allow the discharge record to go straight to the GP
- Clarifying key roles and responsibilities related to patient identification processes across clinical and clerical workflows.
- Monitoring the use of appropriate electronic communication platforms
- Release of the new communication boards to all wards
Achievements and Opportunities
We are proud of…
- Refocusing on use of ISOBAR/ ISBAR in handover processes through an updated Clinical Handover PPG and accompanying WeLearn module extended to all staff
- Use of EMR data as part of dashboards to inform patient care in timely manner (e.g. overdue cannulae)
- The extensive and active involvement of Language Services across Western Health to ensure patients and their carers and families are kept informed about clinical care and treatment planning
- EMR 2.1 GoLive in July which brings clinical services into the one EMR to increase visibility of the patient journey and to reduce fragmentation of information (reducing hybrid workflows)
- Updating ‘What Goes Where’ staff resources as we transition from current systems to the EMR to help staff navigate to the relevant source of information to ensure they have the full picture
- Re-establishing routine audits (eg Consent, Handover) to inform improvement approaches
- Updating and standardizing patient communication boards across WH
- Supporting staff to publish ward round information on EMR in a more timely and effective manner.
We are looking forward to…
- Further developing KHWD boards in clinical areas to share achievements, areas of improvement with patients/ relatives and staff.
- The introduction of the replacement interface to allow discharge summaries to be sent directly to GPs.
Our focus continues on…
- Developing Clinical Handover PPG and Welearn packages to support the exchange of clinical information.
- Re-establishing audits (Patient ID, Consent, Time-Out) to inform improvement approaches.
- Reviewing Riskman data to identify themes of communication incidents to strengthen WH clinical communication capability.
- Continuing to uplift discharge summary sharing with GPs and external health services/ sharing of clinical information between WH and BM&M sites which supports continuity of care.
What our Data Tells Us
Patient Identification
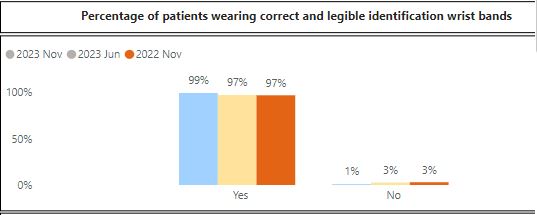
Patient identification is crucial for providing safe and effective healthcare. It ensures that each individual receives the right care, medications, and treatments, while minimising the risk of errors.
Patient wrist bands play a key role in correct identification and procedure matching.
Results from the November 2023 Advancing Best Care (ABC) Audit showed that 99% of patients on audit day were wearing correct and legible identification wrist bands.
Clinical Handover
Clinical handovers are vital for patient safety. They enable clinicians to exchange critical information about a patient’s condition, treatment, and needs when there is a change of staff shift or transitioning care. Effective handovers ensure continuity and prevent mistakes.
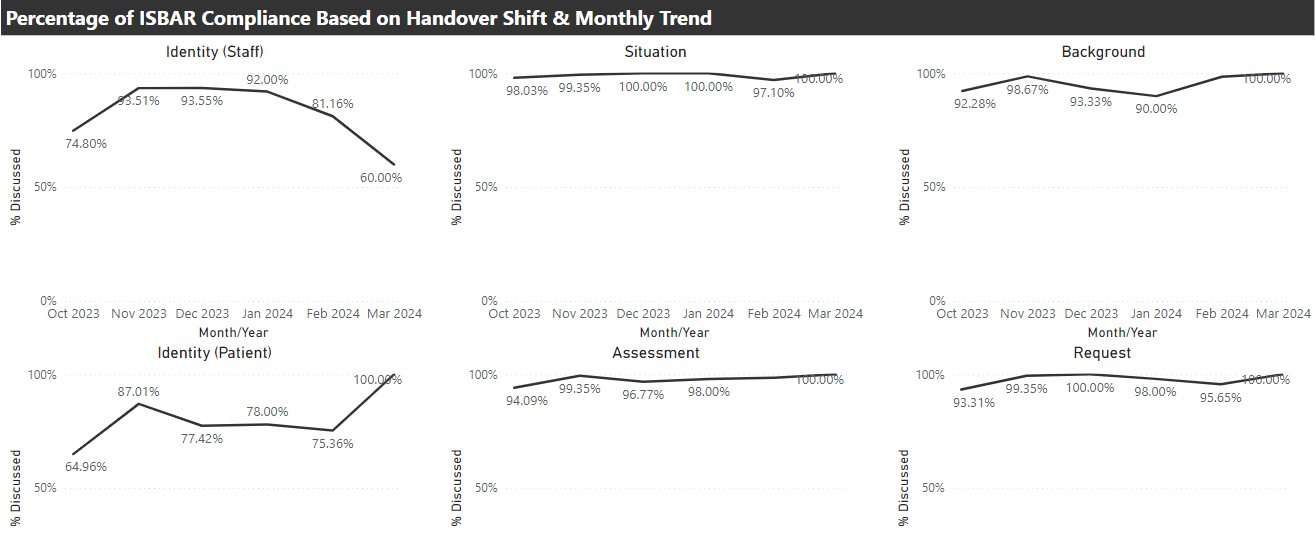
The ISBAR tool is a valuable asset in clinical handovers. It stands for Identify, Situation, Background, Assessment and Request. Western Health uses ISBAR to help clinicians communicate efficiently and ensures crucial information is passed accurately. It’s a simple but effective way to support best care. Following expansion of the use of our Electronic Medical Record (EMR), more staff and services are supported to consistently apply the principles of ISBAR to clinical handovers.
Clinical handover auditing shows good use of ISBAR.
Discharge Planning
Discharge planning and communications are essential for best care. They help ensure a smooth transition from the hospital to home or another care setting. By coordinating post-hospital care and medications, it enhances patient recovery, reduces readmissions, and promotes overall well-being. In essence, discharge planning is a key part of comprehensive and effective healthcare.
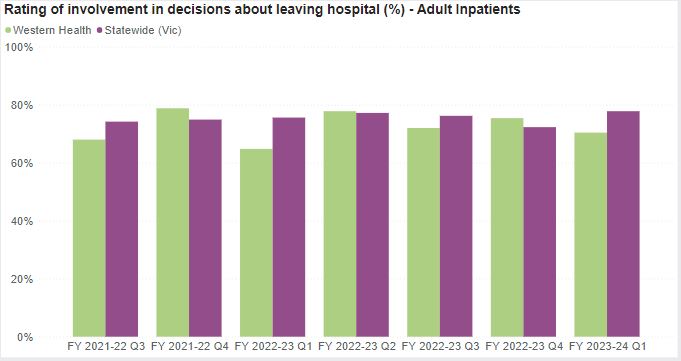
The Victorian Health Experience Survey (VHES) includes patient feedback on planning for discharge from our inpatient services. The Department of Health and Human Services has a target of 75% of very positive responses to questions on discharge care.
The following graph shows the percentage of our patients who provided very positive responses to questions on discharge planning, care and communication to end September 2023. Our results tend to fluctuate between being above and below the Statewide average
Western Health continues to upload patient information to the My Health Record to the Australian My Health Record, a secure and centralised online system storing important health information for consumers. The Australian Digital Health Agency has launched its first consumer mobile application (’My Health’), which enables users to more easily access My Health Record information.
At a local level, Western Health continues to explore better ways of sharing health care information with the General Practitioners (GPs) of consumers using our health care services.