NSQHS: Standard 7: BLOOD MANAGEMENT BULLETIN APRIL | 2024
-
Introducing the Blood Management 'Fab 5'
The ‘Fab 5’ is a team of multi-disciplinary leads brought together to support ongoing National Safety & Quality Health Service (NSQHS) Standard compliance.
The Fab 5 Team for NSQHS Std 7 is:
- Team Lead: Michelle Read
- Quality Lead: Maria Scoles
- Education Lead: Jim Bau
- Professional Leads: Michelle Read (Nursing); Bill Renwick (Medical)
- Subject Matter Experts: Krystel Uy Kimpang, Helen Tran, Linda Williams
-
Do you have any questions?
For any queries about Blood Management you’d like to direct to the NSQHS Std 7 Fab 5 or others, please contact BestCare@wh.org.au
-
Like to know more about Accreditation Readiness?
Visit our Live Best Care site at https://westerly.wh.org.au/livebestcare/ or use the following QR Code to find out more about NSQHS Standard Readiness.

From Michelle

As part of BAU Accreditation Readiness activity, a NSQHS Standard of the Month program has been introduced. This involves a focus on one Standard per month, with communications and walkarounds to help staff be aware of how Best Care at Western Health reflects this Standard, to ask staff possible Surveyor questions and answers, and to walk in a Surveyor’s shoes to see what WH practice looks like.
We are excited that NSQHS Standard 7: Blood Management is to be the focus of the second Standard of the month. This will run from Tuesday 2 April to Friday 26 April. Look out for friendly Fab 5 team members, Best Care Co-ordinators, and other staff who will visit clinical areas/departments to discuss Blood Management with you.
During the month, we will also have a specific focus (with prizes) on all things blood.
Our ‘Fab 5’ team includes blood management CNCs, nursing, medical, education, and quality expertise to support our ongoing compliance with NSQHS Standard 7 – Blood Management.
The good news is we are already providing Best Care and living up to the requirements of NSQHS Std 7 in our everyday work! It is why we performed so well at the December 2023 Accreditation Survey.
Please continue reading to find out more about our Blood Management strategies, achievements and opportunities for improvement, as well as resources to help you to continue to be Accreditation Ready for NSQHS Standard 7.
Michelle Read
NSQHS Std 7 ‘Fab 5’ Team Lead
Director of Nursing & Midwifery
Our approach to Communicating for Safety
The NSQHS Standard 7 – Blood Management Standard aims to ensure patients’ own blood is safely and appropriately managed, and that any blood and blood products that patients receive are safe and appropriate.
Programs and strategies to help support Blood Management at Western Health include:
- Informed patient consent for blood and blood products
- Use of key performance indicators, incident and adverse reaction reporting, and audits to review and enhance blood and blood product management
- Blood and blood product policies, procedures and protocols which support clinical practice in line with National Patient Blood Management Guidelines
- Participation in the Victorian State Haemovigilance Reporting Scheme.
- Blood product and transfusion medicine educational resources for clinical and ancillary staff
- Optimisation and conservation of patient’s own blood
- Equipment and processes to minimise blood and blood product wastage
Resource Centre
The following resources have been put together to support staff to be aware of the NSQHS Blood Management Standard and Accreditation Ready for Survey against this Standard:
- NSQHS Standard 7 Accreditation Walkaround Questions and Answers
- Spotlight on Blood Management – Know Your Standard
- Health Standards (NSQHS) WeLearn Module
Consumer Story

“Our family live in regional Victoria and have two young boys. Over the past decade, we have seen and benefited from the generosity of so many Australians through life-saving blood donation. Throughout this time, we have received large amounts of blood products, in a range of healthcare settings in both regional and metropolitan Victoria.
Over the years, I have had several health concerns which have required multiple transfusions of red blood cells, plasma and platelets. These transfusions have saved my life.
I also suffered significant blood loss during the birth of our two boys, as both were born extremely premature. During the course of my pregnancies, I had several antenatal bleeds which required anti-D injections to prevent haemolytic disease of the newborn which could have been life-threatening to my boys.
When our oldest boy was born at 27 weeks, he required multiple blood transfusions during his stay in the Neonatal intensive care unit (NICU). Following his admission, he continued to have ongoing health concerns as a result of his premature birth.
Our second boy was born at the beginning of the COVID-19 pandemic at just 23 weeks, and like his older brother, he has had significant health issues due to his premature birth. Over his life, he has received in excess of 40 blood transfusions, over 15 transfusions of platelets and plasma, as well as multiple iron transfusions.
Since the birth of our two boys, our family has spent several extended periods of time separated from one another. During this time, many of our family and friends would ask us what they could do to help. Generally, we would politely decline, but then we thought of something they could do – not just for our family but for so many others like us – they could give blood.
My husband and I decided to create a team so our friends and family could support our boys and the countless other recipients in need. Many of our team members have expressed how thankful they are for us encouraging them to get back into donating or starting to donate. We even had family and friends send us photos during their donation, letting us know they were doing this for our boys. Seeing and hearing these things each time a team member donates, brings us so much joy. Knowing that their selfless actions and generosity are literally saving lives, and making a difference to so many people and their families, fills us with gratitude.
For a while, being home together as a family of four, didn’t look like it was going to be a reality for us, but with the help of countless individuals, including generous blood donors, it is the reality we are now living. There are no words to express just how grateful we are to each and every person who has ever donated. Regardless of how many or how few donations a person has been able to make, these donations have changed and saved lives.”
Improvement Initiatives
There are multiple improvement initiatives underway to improve Blood Management. Do you know about these?
- Mandatory training on We learn.
- Blood Champion portfolio initiative
- Patient experience and understanding of consent surveys
- Transfusion alert cards & information pamphlets
- Subcutaneous Immunoglobulin business case
- Advanced scope of practice course for applicable nursing staff
- New Massive Transfusion Protocol audit in collaboration with the Anaesthetics Department
- Use of Multi-Unit Transporters and shippers for blood products to prevent blood wastage
- Communication boards in patient facing spaces across all sites
- Managing Blood Transfusion reactions – procedure for clinical staff.
- Correct patient identification checks.
Achievements and Opportunities
We are proud of …
- Completion of Blood Safety mandatory training increasing across the health service.
- Embedding Blood safety training into all induction programs for medical and nursing staff at Western Health
- The successful amalgamation of all blood processes across Western Health:
- Including the development of multiple new policies to ensure safe and compliant practices
- Removal of all blood products from pharmacy monitored refrigerators, and into blood validated blood refrigerators
- Introduction of a new blood product (Fibrinogen Concentrate) including onsite storage for emergency critical bleeding cases
- Transference of audit results onto the Performance Dashboard – a central platform accessible to all Unit Managers
- Re-introduction of the Blood Management Newsletters following a halt over the Covid-19 pandemic
- Introduction of the Transfusion Alert Cards and information pamphlets for patients with specific transfusion requirements
- Successful roll out of the use of Group O+ red blood cells for patients in meeting a specific criteria, in alignment with the National Blood Authority’s recommendations
- Establishing safe processes for changes of patient ID details in the context of the massive transfusion protocol.
We are looking forward to …
- Transitioning to the New Footscray Hospital in 2025
- Establishing meaningful improvements following the Patient experience and understanding of consent to blood transfusions
- The update of the WeLearn Blood management module – with an anticipated increase in clinician completion rates
- Development and introduction of a Cell Saver Policy, Procedure and Guideline
- Reviewing and improvement blood information sheets provided to patients – including information in different languages
Our focus continues on …
- Providing safe and timely care to patients around all things blood
- Updates around the Massive Transfusion Protocol are appropriate, effective and safe – as MTPs remain a high-risk clinical scenario for the use of blood products
- Ensuring clinicians are well informed on all blood processes, and are aware of the policies and procedures around safe administration
- Identification of high blood users, monitoring of key risk areas and providing targeted education and support for these specialty areas
- Why use 2, when 1 will do campaign
What our Data Tells Us
Wastage of Blood Products
Red blood cells which are prescribed for patients who have clinically significant anaemia – this can be for various underlying reasons. Red blood cells are the most frequently transfused blood product at Western Health.
Donated red blood cell units have a life span of 42 days after which time they cannot be given to patients and must be discarded. For red blood cells that have been manipulated (for example – irradiated), this lifespan shortens.
For this reason, we work very closely with our pathology service providers to continually review the stock (inventory) of blood products keep onsite and rotate our stock as necessary to prevent blood wastage.
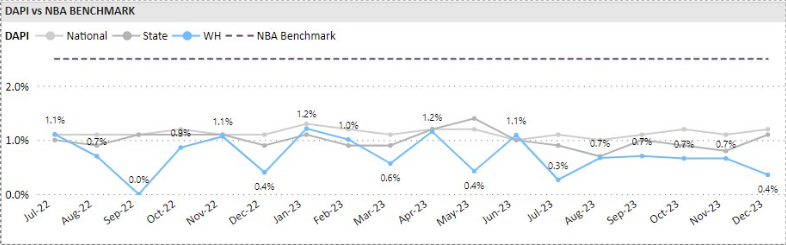
We measure our performance against the State and National discard percentages provided by Lifeblood monthly.
Western Health’s red cell unit discard rate is consistently lower than the State and National discard percentages.
Appropriate Use of Blood Products
Australia has one of the safest blood supplies in the world, however the transfusion of blood products is not without risk and can lead to complications and adverse outcomes for patients. Blood transfusions should only be given if the potential clinical benefits outweigh the potential risks to the patient.
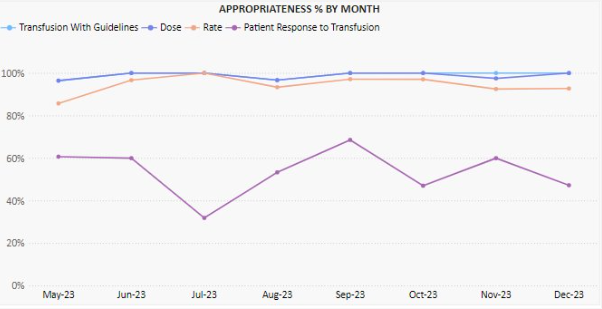
As part of our Blood Management clinical audit program we undertake regular audits of transfusion episodes to review Western Health’s alignment of practice against the National Patient Blood Management Guidelines
Of the two hundred and ninety-nine red cell transfusion episodes audited between May 2023 and December 2023, 99.1% were assessed as being aligned with the National Patient Blood Management Guidelines.
Documentation of Blood Product Administration
One of the NSQHS Standard 7 criterion ensures that the documentation relating to all blood products can be traced from vein (donor) to vein (recipient).
As part of our Blood Management clinical audit program, we undertake regular audits of transfusion episodes to review Western Health’s alignment of practice against the National Patient Blood Management Guidelines
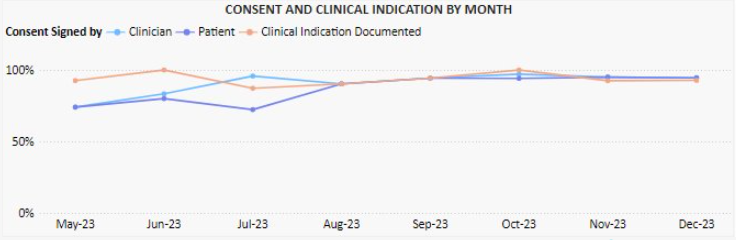
These audits are performed monthly, and monitor:
- Documentation of informed consent
- Documentation of transfusion details (i.e., batch number, start/stop times and date, authorised checkers etc)
- Documentation of cold chain (for remote blood refrigerators)
Of the two hundred and ninety-nine red cell transfusion episodes audited between May 2023 and December 2023, 83.3% had clinical indication for transfusion documented. Over the same time period, documented signing of consent to transfusion by both clinicians and patients has significantly improved.