NSQHS Standard Accreditation Notification
NSQHS Std of the Month: Blood Management


As part of BAU Accreditation Readiness activity, a NSQHS Standard of the Month program has been introduced. This involves a focus on one Standard per month, with communications and walkarounds to help staff be aware of how Best Care at Western Health reflects this Standard, to ask staff possible Surveyor questions and answers, and to walk in a Surveyor’s shoes to see what WH practice looks like.
We are excited that NSQHS Standard 7: Blood Management is to be the focus of the second Standard of the month. This will run from Tuesday 2 April to Friday 26 April. Look out for friendly Fab 5 team members, Best Care Co-ordinators, and other staff who will visit clinical areas/departments to discuss Blood Management with you.
During the month, we will also have a specific focus (with prizes) on all things blood.
Our ‘Fab 5’ team includes blood management CNCs, nursing, medical, education, and quality expertise to support our ongoing compliance with NSQHS Standard 7 – Blood Management.
The good news is we are already providing Best Care and living up to the requirements of NSQHS Std 7 in our everyday work! It is why we performed so well at the December 2023 Accreditation Survey.
Please continue reading to find out more about our Blood Management strategies, achievements and opportunities for improvement, as well as resources to help you to continue to be Accreditation Ready for NSQHS Standard 7.
Michelle Read
NSQHS Std 7 ‘Fab 5’ Team Lead
Director of Nursing & Midwifery
The NSQHS Standard 7 – Blood Management Standard aims to ensure patients’ own blood is safely and appropriately managed, and that any blood and blood products that patients receive are safe and appropriate.
Programs and strategies to help support Blood Management at Western Health include:
- Informed patient consent for blood and blood products
- Use of key performance indicators, incident and adverse reaction reporting, and audits to review and enhance blood and blood product management
- Blood and blood product policies, procedures and protocols which support clinical practice in line with National Patient Blood Management Guidelines
- Participation in the Victorian State Haemovigilance Reporting Scheme.
- Blood product and transfusion medicine educational resources for clinical and ancillary staff
- Optimisation and conservation of patient’s own blood
- Equipment and processes to minimise blood and blood product wastage
The following resources have been put together to support staff to be aware of the NSQHS Blood Management Standard and Accreditation Ready for Survey against this Standard:
- NSQHS Standard 7 Accreditation Walkaround Questions and Answers
- Spotlight on Blood Management – Know Your Standard
- Health Standards (NSQHS) WeLearn Module

“Our family live in regional Victoria and have two young boys. Over the past decade, we have seen and benefited from the generosity of so many Australians through life-saving blood donation. Throughout this time, we have received large amounts of blood products, in a range of healthcare settings in both regional and metropolitan Victoria.
Over the years, I have had several health concerns which have required multiple transfusions of red blood cells, plasma and platelets. These transfusions have saved my life.
I also suffered significant blood loss during the birth of our two boys, as both were born extremely premature. During the course of my pregnancies, I had several antenatal bleeds which required anti-D injections to prevent haemolytic disease of the newborn which could have been life-threatening to my boys.
When our oldest boy was born at 27 weeks, he required multiple blood transfusions during his stay in the Neonatal intensive care unit (NICU). Following his admission, he continued to have ongoing health concerns as a result of his premature birth.
Our second boy was born at the beginning of the COVID-19 pandemic at just 23 weeks, and like his older brother, he has had significant health issues due to his premature birth. Over his life, he has received in excess of 40 blood transfusions, over 15 transfusions of platelets and plasma, as well as multiple iron transfusions.
Since the birth of our two boys, our family has spent several extended periods of time separated from one another. During this time, many of our family and friends would ask us what they could do to help. Generally, we would politely decline, but then we thought of something they could do – not just for our family but for so many others like us – they could give blood.
My husband and I decided to create a team so our friends and family could support our boys and the countless other recipients in need. Many of our team members have expressed how thankful they are for us encouraging them to get back into donating or starting to donate. We even had family and friends send us photos during their donation, letting us know they were doing this for our boys. Seeing and hearing these things each time a team member donates, brings us so much joy. Knowing that their selfless actions and generosity are literally saving lives, and making a difference to so many people and their families, fills us with gratitude.
For a while, being home together as a family of four, didn’t look like it was going to be a reality for us, but with the help of countless individuals, including generous blood donors, it is the reality we are now living. There are no words to express just how grateful we are to each and every person who has ever donated. Regardless of how many or how few donations a person has been able to make, these donations have changed and saved lives.”
There are multiple improvement initiatives underway to improve Blood Management. Do you know about these?
- Mandatory training on We learn.
- Blood Champion portfolio initiative
- Patient experience and understanding of consent surveys
- Transfusion alert cards & information pamphlets
- Subcutaneous Immunoglobulin business case
- Advanced scope of practice course for applicable nursing staff
- New Massive Transfusion Protocol audit in collaboration with the Anaesthetics Department
- Use of Multi-Unit Transporters and shippers for blood products to prevent blood wastage
- Communication boards in patient facing spaces across all sites
- Managing Blood Transfusion reactions – procedure for clinical staff.
- Correct patient identification checks.
We are proud of …
- Completion of Blood Safety mandatory training increasing across the health service.
- Embedding Blood safety training into all induction programs for medical and nursing staff at Western Health
- The successful amalgamation of all blood processes across Western Health:
- Including the development of multiple new policies to ensure safe and compliant practices
- Removal of all blood products from pharmacy monitored refrigerators, and into blood validated blood refrigerators
- Introduction of a new blood product (Fibrinogen Concentrate) including onsite storage for emergency critical bleeding cases
- Transference of audit results onto the Performance Dashboard – a central platform accessible to all Unit Managers
- Re-introduction of the Blood Management Newsletters following a halt over the Covid-19 pandemic
- Introduction of the Transfusion Alert Cards and information pamphlets for patients with specific transfusion requirements
- Successful roll out of the use of Group O+ red blood cells for patients in meeting a specific criteria, in alignment with the National Blood Authority’s recommendations
- Establishing safe processes for changes of patient ID details in the context of the massive transfusion protocol.
We are looking forward to …
- Transitioning to the New Footscray Hospital in 2025
- Establishing meaningful improvements following the Patient experience and understanding of consent to blood transfusions
- The update of the WeLearn Blood management module – with an anticipated increase in clinician completion rates
- Development and introduction of a Cell Saver Policy, Procedure and Guideline
- Reviewing and improvement blood information sheets provided to patients – including information in different languages
Our focus continues on …
- Providing safe and timely care to patients around all things blood
- Updates around the Massive Transfusion Protocol are appropriate, effective and safe – as MTPs remain a high-risk clinical scenario for the use of blood products
- Ensuring clinicians are well informed on all blood processes, and are aware of the policies and procedures around safe administration
- Identification of high blood users, monitoring of key risk areas and providing targeted education and support for these specialty areas
- Why use 2, when 1 will do campaign
Wastage of Blood Products
Red blood cells which are prescribed for patients who have clinically significant anaemia – this can be for various underlying reasons. Red blood cells are the most frequently transfused blood product at Western Health.
Donated red blood cell units have a life span of 42 days after which time they cannot be given to patients and must be discarded. For red blood cells that have been manipulated (for example – irradiated), this lifespan shortens.
For this reason, we work very closely with our pathology service providers to continually review the stock (inventory) of blood products keep onsite and rotate our stock as necessary to prevent blood wastage.
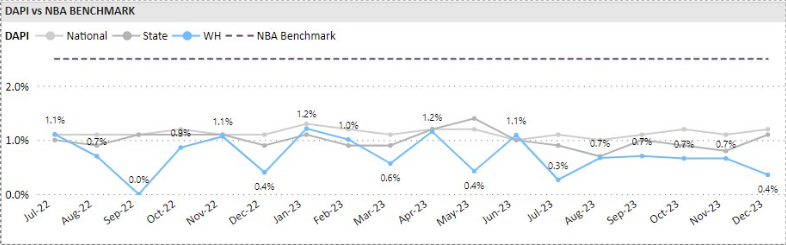
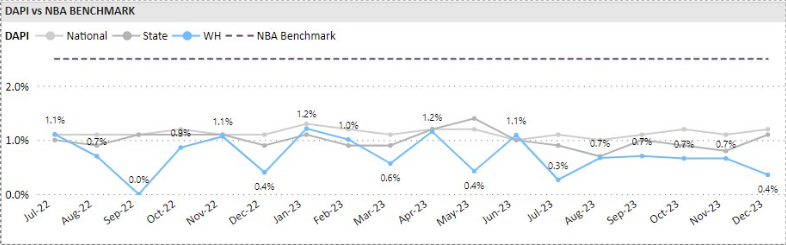
We measure our performance against the State and National discard percentages provided by Lifeblood monthly.
Western Health’s red cell unit discard rate is consistently lower than the State and National discard percentages.
Appropriate Use of Blood Products
Australia has one of the safest blood supplies in the world, however the transfusion of blood products is not without risk and can lead to complications and adverse outcomes for patients. Blood transfusions should only be given if the potential clinical benefits outweigh the potential risks to the patient.
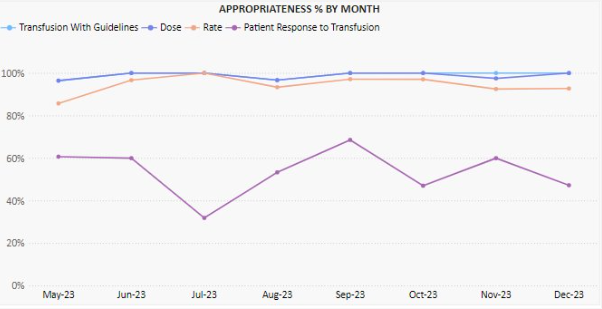
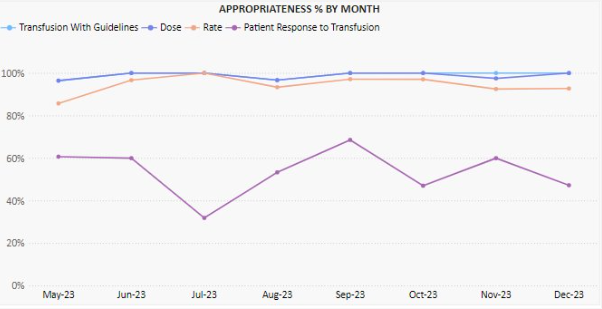
As part of our Blood Management clinical audit program we undertake regular audits of transfusion episodes to review Western Health’s alignment of practice against the National Patient Blood Management Guidelines
Of the two hundred and ninety-nine red cell transfusion episodes audited between May 2023 and December 2023, 99.1% were assessed as being aligned with the National Patient Blood Management Guidelines.
Documentation of Blood Product Administration
One of the NSQHS Standard 7 criterion ensures that the documentation relating to all blood products can be traced from vein (donor) to vein (recipient).
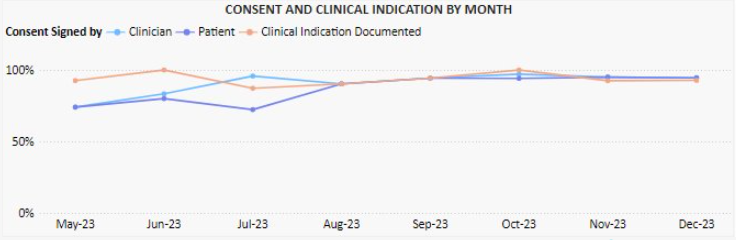
As part of our Blood Management clinical audit program, we undertake regular audits of transfusion episodes to review Western Health’s alignment of practice against the National Patient Blood Management Guidelines
These audits are performed monthly, and monitor:
- Documentation of informed consent
- Documentation of transfusion details (i.e., batch number, start/stop times and date, authorised checkers etc)
- Documentation of cold chain (for remote blood refrigerators)
Of the two hundred and ninety-nine red cell transfusion episodes audited between May 2023 and December 2023, 83.3% had clinical indication for transfusion documented. Over the same time period, documented signing of consent to transfusion by both clinicians and patients has significantly improved.
The latest benchmark reports from the Health Roundtable that go up to September 2023 have recently been released, that show how our delivery of Best Care compares to other health services across Australasia.
Let’s look at how we perform in the area of Medication complications, which include drug related respiratory complications/depression, haemorrhagic disorder due to circulating anticoagulants, movement disorders due to psychotropic medication and serious alteration to conscious state due to psychotropic medication.
Medication Complications:
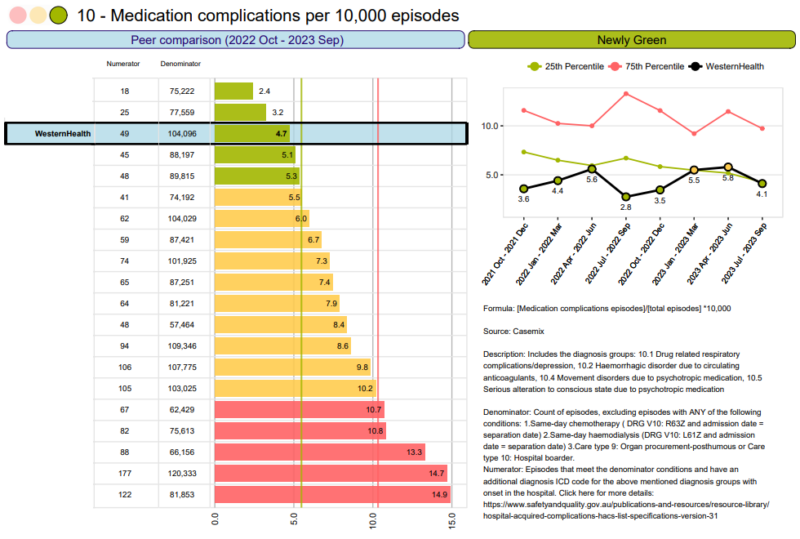
At Western Health as a whole the rates of medication complications per 10,000 episodes has been consistently green. We are amongst some of the best outcomes in Australia. This is a wonderful result.
The last quarter this has decreased again to green.
Well done to all of our Western Health teams.
National Close the Gap Day was recently held on 21 March 2024, and recognises the national agreement to overcome inequality experienced by Aboriginal and Torres Strait Islander people and achieve life outcomes equal to non-Indigenous Australians.
Aboriginal and Torres Strait Islander people and achieve life outcomes equal to non-Indigenous Australians.
Each year progress on the 19 national socio-economic targets across areas that have an impact on life outcomes for Aboriginal and Torres Strait Islander people is reported.
They range from ensuring babies are born at a healthy birthweight, supporting children to thrive, and ensuring there are appropriate pathways for education and employment.
Progress has been made, but it has been too slow and the gap is still too wide. For instance, Aboriginal and Torres Strait Islander people still have a life expectancy that is 10-11 years less than non-Indigenous Australians!
Western Health has a growing Aboriginal and Torres Strait Islander community and is committed to self-determination. As part of our efforts to close the gap we are incredibly proud of the culturally responsive care options we have designed to ensure that Aboriginal and Torres Strait Islander patients receive respectful, high-quality care with greater access and choice. These include:
- The Galinjera Maternity Program
A small team of dedicated midwives and doctors, who provide culturally-safe continuous care to Aboriginal and Torres Strait Islander families and babies. You can read more about how this service is improving outcomes for our community on our website.
- Babaneek Booboop Program
A program promoting the health and developmental outcomes of First Nations children in Melbourne’s Western Suburbs (the City of Melton and Moorabool Shire). Establishing and building on strong networks, the program supports children and their families in their engagement with child health and promotes cultural safety in health.
It won the Excellence in Aboriginal Health and Wellbeing Award at the Victorian Public Healthcare Awards in 2023. Read more.
- The Aboriginal and Torres Strait Islander Outpatient Clinic
A culturally safe, general medicine stream clinic for Aboriginal and Torres Strait Islander adults with chronic health conditions who do not require urgent care.
It is designed to provide a wrap-around service for patients with longer appointment times, a multidisciplinary focus, assistance with any barriers to attending and the individualised support and advocacy of an Aboriginal Hospital Liaison Officer (AHLO). Read more.
Wilim Berrbang Manager (Acting) Ashleigh Vandenberg and Wiradjuri woman said that everyone has a part to play in helping us achieve health equity for all Australians. “We all have a role to play in closing the gap and our actions can have a positive impact on the health and wellbeing of Aboriginal and Torres Strait Islanders and society more broadly,” Ashleigh said.
New support for Aboriginal Menal Health consumers

To improve the way we support consumers and their families seeking support with their mental health and wellbeing, Western Health has appointed our first Aboriginal Mental Health Liaison Officer in Wilim Berrbang.
Maddie DePetro (pictured right) is from the Yorta Yorta & Dja Dja Warrung clan and is passionate about ensuring Aboriginal and Torres Strait Islander patients feel heard within the healthcare system.
Referrals can be made to Maddie via the Wilim.Berrbang@wh.org.au, via phone on 0482 130 724, or on EMR select: Aboriginal health- Other- Request AMHLO support.
How can I make a difference?
You can make a difference by being educated and informed on ways you can provide culturally-safe care:
- Read more about Closing the Gap on its website. The latest report was released on 21 March.
- Read Western Health’s Cultural Safety Plan.
- Complete our cultural awareness training on WeLearn to improve your understanding of Aboriginal and Torres Strait Islander cultures, histories and successes.
- Visit the Wilim Berrbang team staff intranet page.
The current shortage of IV Paracetamol 1000mg/100mL vials/bag in Australia is anticipated to continue until June 2024 due to unexpected increase in demand and production delays.
increase in demand and production delays.
Clinicians are requested to consider alternative routes of administration and to reserve the use of IV vials for situations where alternative routes are not suitable.
Western Health has limited stock available, and hence usage of stock is being monitored closely. Over the past week usage of this product has not reduced sufficiently despite various interventions, and subsequently our projected stock holdings continue to decline. Hence, we are now taking the measure of removing stock from additional Western Health imprest sites except for ICU, Theatre and Emergency Department locations.
Paracetamol suppositories have been added to all imprests currently/previously stocking IV preparations and should be used as a first-line alternative for patients unable to have oral preparations.
Please contact Pharmacy for individual requests for paracetamol IV supply in locations where it has been removed from imprest.


As part of BAU Accreditation Readiness activity, a NSQHS Standard of the Month program has been introduced. This involves a focus on one Standard per month, with communications and walkarounds to help staff be aware of how Best Care at Western Health reflects this Standard, to ask staff possible Surveyor questions and answers, and to walk in a Surveyor’s shoes to see what WH practice looks like.
We are excited that NSQHS Standard 7: Blood Management is to be the focus of the second Standard of the month. This will run from Tuesday 2 April to Friday 26 April. Look out for friendly Fab 5 team members, Best Care Co-ordinators, and other staff who will visit clinical areas/departments to discuss Blood Management with you.
During the month, we will also have a specific focus (with prizes) on all things blood.
Our ‘Fab 5’ team includes blood management CNCs, nursing, medical, education, and quality expertise to support our ongoing compliance with NSQHS Standard 7 – Blood Management.
The good news is we are already providing Best Care and living up to the requirements of NSQHS Std 7 in our everyday work! It is why we performed so well at the December 2023 Accreditation Survey.
Please continue reading to find out more about our Blood Management strategies, achievements and opportunities for improvement, as well as resources to help you to continue to be Accreditation Ready for NSQHS Standard 7.
Michelle Read
NSQHS Std 7 ‘Fab 5’ Team Lead
Director of Nursing & Midwifery
The NSQHS Standard 7 – Blood Management Standard aims to ensure patients’ own blood is safely and appropriately managed, and that any blood and blood products that patients receive are safe and appropriate.
Programs and strategies to help support Blood Management at Western Health include:
- Informed patient consent for blood and blood products
- Use of key performance indicators, incident and adverse reaction reporting, and audits to review and enhance blood and blood product management
- Blood and blood product policies, procedures and protocols which support clinical practice in line with National Patient Blood Management Guidelines
- Participation in the Victorian State Haemovigilance Reporting Scheme.
- Blood product and transfusion medicine educational resources for clinical and ancillary staff
- Optimisation and conservation of patient’s own blood
- Equipment and processes to minimise blood and blood product wastage
The following resources have been put together to support staff to be aware of the NSQHS Blood Management Standard and Accreditation Ready for Survey against this Standard:
- NSQHS Standard 7 Accreditation Walkaround Questions and Answers
- Spotlight on Blood Management – Know Your Standard
- Health Standards (NSQHS) WeLearn Module

“Our family live in regional Victoria and have two young boys. Over the past decade, we have seen and benefited from the generosity of so many Australians through life-saving blood donation. Throughout this time, we have received large amounts of blood products, in a range of healthcare settings in both regional and metropolitan Victoria.
Over the years, I have had several health concerns which have required multiple transfusions of red blood cells, plasma and platelets. These transfusions have saved my life.
I also suffered significant blood loss during the birth of our two boys, as both were born extremely premature. During the course of my pregnancies, I had several antenatal bleeds which required anti-D injections to prevent haemolytic disease of the newborn which could have been life-threatening to my boys.
When our oldest boy was born at 27 weeks, he required multiple blood transfusions during his stay in the Neonatal intensive care unit (NICU). Following his admission, he continued to have ongoing health concerns as a result of his premature birth.
Our second boy was born at the beginning of the COVID-19 pandemic at just 23 weeks, and like his older brother, he has had significant health issues due to his premature birth. Over his life, he has received in excess of 40 blood transfusions, over 15 transfusions of platelets and plasma, as well as multiple iron transfusions.
Since the birth of our two boys, our family has spent several extended periods of time separated from one another. During this time, many of our family and friends would ask us what they could do to help. Generally, we would politely decline, but then we thought of something they could do – not just for our family but for so many others like us – they could give blood.
My husband and I decided to create a team so our friends and family could support our boys and the countless other recipients in need. Many of our team members have expressed how thankful they are for us encouraging them to get back into donating or starting to donate. We even had family and friends send us photos during their donation, letting us know they were doing this for our boys. Seeing and hearing these things each time a team member donates, brings us so much joy. Knowing that their selfless actions and generosity are literally saving lives, and making a difference to so many people and their families, fills us with gratitude.
For a while, being home together as a family of four, didn’t look like it was going to be a reality for us, but with the help of countless individuals, including generous blood donors, it is the reality we are now living. There are no words to express just how grateful we are to each and every person who has ever donated. Regardless of how many or how few donations a person has been able to make, these donations have changed and saved lives.”
There are multiple improvement initiatives underway to improve Blood Management. Do you know about these?
- Mandatory training on We learn.
- Blood Champion portfolio initiative
- Patient experience and understanding of consent surveys
- Transfusion alert cards & information pamphlets
- Subcutaneous Immunoglobulin business case
- Advanced scope of practice course for applicable nursing staff
- New Massive Transfusion Protocol audit in collaboration with the Anaesthetics Department
- Use of Multi-Unit Transporters and shippers for blood products to prevent blood wastage
- Communication boards in patient facing spaces across all sites
- Managing Blood Transfusion reactions – procedure for clinical staff.
- Correct patient identification checks.
We are proud of …
- Completion of Blood Safety mandatory training increasing across the health service.
- Embedding Blood safety training into all induction programs for medical and nursing staff at Western Health
- The successful amalgamation of all blood processes across Western Health:
- Including the development of multiple new policies to ensure safe and compliant practices
- Removal of all blood products from pharmacy monitored refrigerators, and into blood validated blood refrigerators
- Introduction of a new blood product (Fibrinogen Concentrate) including onsite storage for emergency critical bleeding cases
- Transference of audit results onto the Performance Dashboard – a central platform accessible to all Unit Managers
- Re-introduction of the Blood Management Newsletters following a halt over the Covid-19 pandemic
- Introduction of the Transfusion Alert Cards and information pamphlets for patients with specific transfusion requirements
- Successful roll out of the use of Group O+ red blood cells for patients in meeting a specific criteria, in alignment with the National Blood Authority’s recommendations
- Establishing safe processes for changes of patient ID details in the context of the massive transfusion protocol.
We are looking forward to …
- Transitioning to the New Footscray Hospital in 2025
- Establishing meaningful improvements following the Patient experience and understanding of consent to blood transfusions
- The update of the WeLearn Blood management module – with an anticipated increase in clinician completion rates
- Development and introduction of a Cell Saver Policy, Procedure and Guideline
- Reviewing and improvement blood information sheets provided to patients – including information in different languages
Our focus continues on …
- Providing safe and timely care to patients around all things blood
- Updates around the Massive Transfusion Protocol are appropriate, effective and safe – as MTPs remain a high-risk clinical scenario for the use of blood products
- Ensuring clinicians are well informed on all blood processes, and are aware of the policies and procedures around safe administration
- Identification of high blood users, monitoring of key risk areas and providing targeted education and support for these specialty areas
- Why use 2, when 1 will do campaign
Wastage of Blood Products
Red blood cells which are prescribed for patients who have clinically significant anaemia – this can be for various underlying reasons. Red blood cells are the most frequently transfused blood product at Western Health.
Donated red blood cell units have a life span of 42 days after which time they cannot be given to patients and must be discarded. For red blood cells that have been manipulated (for example – irradiated), this lifespan shortens.
For this reason, we work very closely with our pathology service providers to continually review the stock (inventory) of blood products keep onsite and rotate our stock as necessary to prevent blood wastage.
We measure our performance against the State and National discard percentages provided by Lifeblood monthly.
Western Health’s red cell unit discard rate is consistently lower than the State and National discard percentages.
Appropriate Use of Blood Products
Australia has one of the safest blood supplies in the world, however the transfusion of blood products is not without risk and can lead to complications and adverse outcomes for patients. Blood transfusions should only be given if the potential clinical benefits outweigh the potential risks to the patient.
As part of our Blood Management clinical audit program we undertake regular audits of transfusion episodes to review Western Health’s alignment of practice against the National Patient Blood Management Guidelines
Of the two hundred and ninety-nine red cell transfusion episodes audited between May 2023 and December 2023, 99.1% were assessed as being aligned with the National Patient Blood Management Guidelines.
Documentation of Blood Product Administration
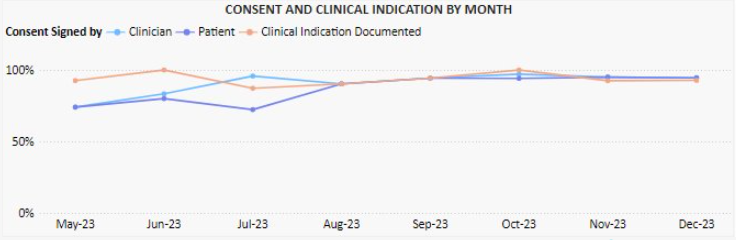
One of the NSQHS Standard 7 criterion ensures that the documentation relating to all blood products can be traced from vein (donor) to vein (recipient).
As part of our Blood Management clinical audit program, we undertake regular audits of transfusion episodes to review Western Health’s alignment of practice against the National Patient Blood Management Guidelines
These audits are performed monthly, and monitor:
- Documentation of informed consent
- Documentation of transfusion details (i.e., batch number, start/stop times and date, authorised checkers etc)
- Documentation of cold chain (for remote blood refrigerators)
Of the two hundred and ninety-nine red cell transfusion episodes audited between May 2023 and December 2023, 83.3% had clinical indication for transfusion documented. Over the same time period, documented signing of consent to transfusion by both clinicians and patients has significantly improved.

The Clinical Communiqué is an electronic publication containing narrative case reports about lessons learned from Coroners’ investigations into preventable deaths in acute hospital and community settings. The Clinical Communiqué is written by clinicians, for clinicians.
Associate Professor Nicola Cunningham
Welcome to the first issue of the Clinical Communiqué for 2024. In this edition we are looking at the challenging aspects of determining fitness to drive in older drivers. Advancing age is associated with co-morbidities that cumulatively increase driving risk and will affect a person’s fitness to drive. Stroke, dementia, sleep disorders, mobility issues, hearing and vision impairment may warrant cessation of driving. The two cases in
this edition demonstrate two main risk profiles in older drivers – the driving risks when a patient is bodily capable but easily disorientated, and the driving risks when a patient is mentally sharp but physically slow. A diagnosis of dementia or a physical impairment does not automatically signify a patient should lose their licence, but it does herald the need for notification to the licensing authority and an assessment of fitness to drive.
This is not the first time The Communiqués team have shared important learnings from coronial cases about fitness to drive. We explored the theme in a previous edition of the Clinical Communiqué (September 2015 Edition Volume 2; Issue 3) where we featured three case summaries and an expert commentary from Australia’s leading forensic medical experts in traffic medicine. The edition highlighted the complexities surrounding driving ability in patients with a range of chronic medical conditions, and the role of their treating practitioners. In those cases, hypoglycaemia, seizures, and visual impairment were each found to be contributing factors in fatal collisions. Associate Professor Morris
Odell’s expert commentary on the complexities of considering fitness to drive in the context of the effect of the condition on the ability to perform the tasks of driving, and the jurisdictional differences in reporting, is as important and relevant today as it was then.
Although the focus this time is on older drivers and how to ensure driving safety in the setting of age-related cognitive and physical changes, the fundamental messages are the same:
1. A person’s suitability to hold a licence is a question that should be asked early in a therapeutic relationship.
2. It is crucial to perform a comprehensive driving assessment with input from multidisciplinary sources about a person’s medical conditions – their abilities and limitations, and their driving history.
3. Legal obligations and licensing guidelines should be understood by all health professionals. As Dr Gaya cogently wrote in the previous fitness to drive edition, “Driving is not a right, but a privilege…subtle effects of a fairly common medical condition in a driver can disastrously
impact on the driver and other road users. For this reason, it is incumbent on both drivers and their healthcare professionals to further extend their therapeutic relationship to consider the impact of their conditions and treatments on driving.”
As well as the importance of understanding the steps involved in assessing driving ability in a patient, health professionals must also appreciate the key impacts of a loss of licence for a patient. It represents a loss of independence, with reduced mobility, confidence and autonomy, potentially leading to social isolation and depression. In employed patients this can also have a negative economic impact.
Dr Angela Sungaila returns in this latest edition with a case summary, and the expert commentary is by another leading expert in the field of fitness to drive, Professor Dimity Pond who is a general practitioner, researcher, and educator with a special interest in dementia.
Professor Pond’s commentary shares insights about fitness to drive in older drivers from the perspective of the patient, the health professional, and the system. Her gentle and proactive approach to the issue is one that we should all adopt for our patients. Don’t avoid the conversations and do explore what assistance and limitations might need to be put in place. Driving is an activity that benefits every one of us, so we all play a role in keeping road users safe.

 As part of BAU Accreditation Readiness activity, a NSQHS Standard of the Month program has been introduced. This involves a focus on one Standard per month, with communications and walkarounds to help staff be aware of how Best Care at Western Health reflects this Standard, to ask staff possible Surveyor questions and answers, and to walk in a Surveyor’s shoes to see what WH practice looks like.
As part of BAU Accreditation Readiness activity, a NSQHS Standard of the Month program has been introduced. This involves a focus on one Standard per month, with communications and walkarounds to help staff be aware of how Best Care at Western Health reflects this Standard, to ask staff possible Surveyor questions and answers, and to walk in a Surveyor’s shoes to see what WH practice looks like.
We are excited that NSQHS Standard 6: Communicating for Safety is to be the focus of the first Standard of the month. This will run from Monday 4 March to Friday 29 March. Look out for friendly Best Care Co-ordinators, Fab 5 team members, and other staff who will visit clinical areas/departments to discuss Communicating for Safety with you.
During the month, we will also have a specific focus on the use of Communication Boards and staff engagement in the new Clinical Handover training module.
The Communicating for Safety Standard aims to ensure there is effective communication between patients, carers and families, multi-disciplinary teams and clinicians, and across the health service organisation, to support continuous, co-ordinated and safe care for patients.
The good news is we are already providing Best Care and living up to the requirements of this Standard in our everyday work! It is why we performed so well in the December 2023 Accreditation Survey.
Please continue reading to find out more about our Communicating for Safety strategies, achievements and opportunities for improvement, as well as resources to help you to continue to be Accreditation Ready for NSQHS Standard 6.
Douglas Mill
NSQHS Std 6 ‘Fab 5’ Team Lead
Director of Nursing & Midwifery
The NSQHS Standard 6 – Communicating for Safety is aimed at improving communication within healthcare organisations and reducing the risk of harm to patients.
Western Health’s comprehensive approach to Communicating for Safety draws upon the requirements of this Standard and supports the monitoring, review and improvement of safe care. Programs and strategies to help support communicating for safety include:
- Communication learning packages to support staff knowledge and use of effective communication techniques.
- Reviewing clinical incidents to look for themes around clinical communication and identify areas for improvement.
- Clinical handover protocols to support good communication between our healthcare teams and clear documentation of patient information.
- The use of an electronic medical record to help ensure patient information is easily accessible and up-to-date, which can improve communication between the healthcare team.
- Key roles and responsibilities related to patient identification processes across clinical and clerical workflows.
The following resources have been put together to support staff to be aware of the NSQHS Comprehensive Care standard and Accreditation Ready for Survey against this Standard:
The following resources have been put together to support staff to be aware of the NSQHS Comprehensive Care standard and Accreditation Ready for Survey against this Standard:
- NSQHS Standard 6 Accreditation Walkaround Questions and Answers
- NSQHS Standards at a Glance
- Health Standards (NSQHS) WeLearn Module

Using ISBAR
After an unexpected death in one of our chronic care services, the family were obviously distressed. Being a very spiritual family the operations manager used the ISBAR process to communicate the need for urgent pastoral care.
The pastoral care manager was able to quickly understand the situation and what was required and had pastoral care support on site with the family within 30 mins.
The family were very grateful for the support in this difficult time.
Using the information provided, the manager recognised that other patients may have been traumatised in the unit and facilitated a pastoral care visit for each of the other 20 patients.
Without the use of ISBAR the urgency of this situation would have been delayed. There is no doubt that it allows fast and accurate transfer of information to ensure our patients and carers receive best care.
There are multiple improvement initiatives underway to improve Communicating for Safety. Do you know about these?
- WeLearn package to set the standard for Clinical Handover has been rewritten to make it contemporary and applicable to all craft groups
- Reviewing clinical incidents to see look for themes around clinical communication to identify areas for improvement continues at every meeting of the committee
- Replacement of the electronic program to allow the discharge record to go straight to the GP
- Clarifying key roles and responsibilities related to patient identification processes across clinical and clerical workflows.
- Monitoring the use of appropriate electronic communication platforms
- Release of the new communication boards to all wards
We are proud of…
- Refocusing on use of ISOBAR/ ISBAR in handover processes through an updated Clinical Handover PPG and accompanying WeLearn module extended to all staff
- Use of EMR data as part of dashboards to inform patient care in timely manner (e.g. overdue cannulae)
- The extensive and active involvement of Language Services across Western Health to ensure patients and their carers and families are kept informed about clinical care and treatment planning
- EMR 2.1 GoLive in July which brings clinical services into the one EMR to increase visibility of the patient journey and to reduce fragmentation of information (reducing hybrid workflows)
- Updating ‘What Goes Where’ staff resources as we transition from current systems to the EMR to help staff navigate to the relevant source of information to ensure they have the full picture
- Re-establishing routine audits (eg Consent, Handover) to inform improvement approaches
- Updating and standardizing patient communication boards across WH
- Supporting staff to publish ward round information on EMR in a more timely and effective manner.
We are looking forward to…
- Further developing KHWD boards in clinical areas to share achievements, areas of improvement with patients/ relatives and staff.
- The introduction of the replacement interface to allow discharge summaries to be sent directly to GPs.
Our focus continues on…
- Developing Clinical Handover PPG and Welearn packages to support the exchange of clinical information.
- Re-establishing audits (Patient ID, Consent, Time-Out) to inform improvement approaches.
- Reviewing Riskman data to identify themes of communication incidents to strengthen WH clinical communication capability.
- Continuing to uplift discharge summary sharing with GPs and external health services/ sharing of clinical information between WH and BM&M sites which supports continuity of care.
Patient Identification
Patient identification is crucial for providing safe and effective healthcare. It ensures that each individual receives the right care, medications, and treatments, while minimising the risk of errors.
Patient wrist bands play a key role in correct identification and procedure matching.
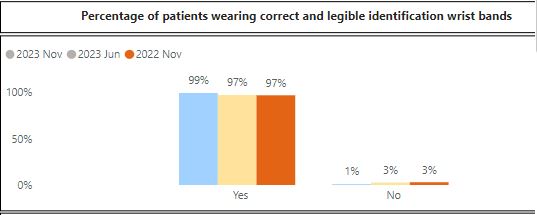
Results from the November 2023 Advancing Best Care (ABC) Audit showed that 99% of patients on audit day were wearing correct and legible identification wrist bands.
Clinical Handover
Clinical handovers are vital for patient safety. They enable clinicians to exchange critical information about a patient’s condition, treatment, and needs when there is a change of staff shift or transitioning care. Effective handovers ensure continuity and prevent mistakes.
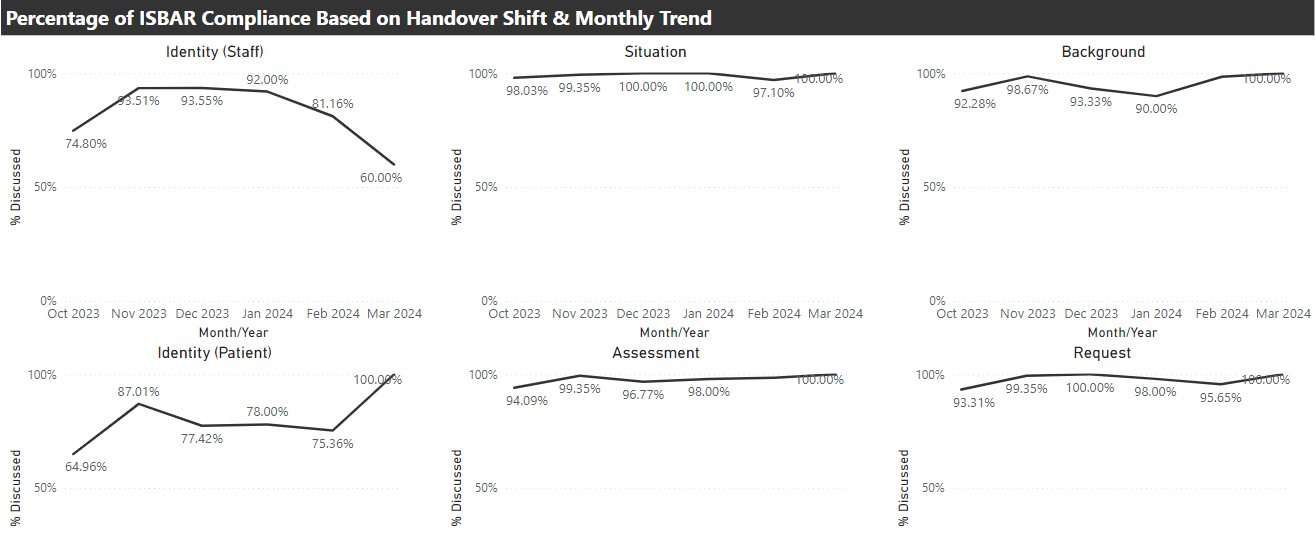
The ISBAR tool is a valuable asset in clinical handovers. It stands for Identify, Situation, Background, Assessment and Request. Western Health uses ISBAR to help clinicians communicate efficiently and ensures crucial information is passed accurately. It’s a simple but effective way to support best care. Following expansion of the use of our Electronic Medical Record (EMR), more staff and services are supported to consistently apply the principles of ISBAR to clinical handovers.
Clinical handover auditing shows good use of ISBAR.
Discharge Planning
Discharge planning and communications are essential for best care. They help ensure a smooth transition from the hospital to home or another care setting. By coordinating post-hospital care and medications, it enhances patient recovery, reduces readmissions, and promotes overall well-being. In essence, discharge planning is a key part of comprehensive and effective healthcare.
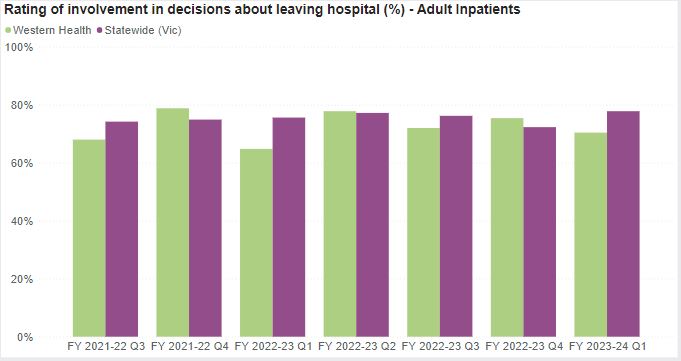
The Victorian Health Experience Survey (VHES) includes patient feedback on planning for discharge from our inpatient services. The Department of Health and Human Services has a target of 75% of very positive responses to questions on discharge care.
The following graph shows the percentage of our patients who provided very positive responses to questions on discharge planning, care and communication to end September 2023. Our results tend to fluctuate between being above and below the Statewide average
Western Health continues to upload patient information to the My Health Record to the Australian My Health Record, a secure and centralised online system storing important health information for consumers. The Australian Digital Health Agency has launched its first consumer mobile application (’My Health’), which enables users to more easily access My Health Record information.
At a local level, Western Health continues to explore better ways of sharing health care information with the General Practitioners (GPs) of consumers using our health care services.

 This edition we would like to acknowledge the FHED and Access teams who received a Best Care award for Coordinated Care in relation to Footscray Short Stay Unit Flow.
This edition we would like to acknowledge the FHED and Access teams who received a Best Care award for Coordinated Care in relation to Footscray Short Stay Unit Flow.
The Short Stay Unit is crucial in achieving the flow required to see new patients in a timely manner. The team identified two interventions to implement in the unit – capping the number of patients admitted to the SSU and allowing better flow by defining criteria for direct admission. By implementing these changes the unit was able to see measurable improvement in the way the SSU ran but also the whole of the ED.


A 72 year old female was admitted to Ward 2C on the 15th September 2023. She had been recently discharged from hospital to a new RACF but represented within 38 hours due to ongoing behavioral issues secondary to a history of Alzheimer’s Disease and Vascular Dementia with Behavioural and Psychological Symptoms of Dementia.
On arrival to the ward, the patient was identified as a high Occupational Violence and Aggression risk and required multiple code greys to manage her behaviours of concerns. Although she had an Additional Care Resource to support her care, her behaviours were challenging for the multidisciplinary team to manage.
A behavioural management plan was developed and included medication reconciliation, planned code greys, use of Greek music and dolls as a distraction. Her family were also involved in the planning of her care. The outcome was positive with better management of her behaviours of concerns.
The patient was transferred to the treating teams home ward several days later, where she became unsettled and had an altercation with another inpatient. She was transferred back to 2C, where her behaviours quickly settled again. This story demonstrates the quality of care provided by the 2C team and highlights their ability to develop relationships and manage difficult behaviours well.
A transfer to the Dementia Management Unit was planned for the patient while work continued on her discharge planning.
Well done to all staff involved in the care of this patient with a complex condition and needs.

“My father was recently admitted to 3E, I understand there was a serious incident, and my father was transferred to Cath lab for the duration of his stay.
There was an in-charge on Saturday morning, who actually did a double shift (not sure her name) and in her hectic day she went above and beyond her job description by keeping me updated regarding my fathers’ management.
I also have to commend an ANUM from 3E who on Sunday took some time and went searching for my father’s missing belongings while coordinating his discharge. She was reassuring in her delivery of care to me.
While we always hear the negative, I want to acknowledge the above as well as all the staff on the ward who took great care and showed compassion to my elderly father. They managed to keep it all together in a frightening situation.
I am proud to say I work for Western Health and how we work not only as a team but a family.
I feel that this needs to be highlighted for all to see.” (From a WH staff member)
There are multiple improvement initiatives underway across EMA. Do you know about these? (If not, feel free to ask your manager).
• Standardised Operating Processes for the Bed Coordinator teams to improve time to allocate beds from ED• Implementation of Virtual communications between our Urgent Care Centres and main Emergency Departments, improving clinical support to Urgent Care
• Ongoing access and flow initiatives across our EDs, including the use of Short Stay Units, AV Offload, Front of House and Fast-Track models, Category 2 time to be seen, use of Lower West Ward at Williamstown
• Comprehensive Care Improvement project across our EDs and Urgent Care Centres, focusing on nursing leadership and risk assessment and tools, including FirstNet implementation/utilisation and revision of audit tools and processes
• Timely Emergency Care Collaborative (TECC) aiming to improve the timeliness of emergency care through improving system-wide patient flow – PDSA cycles continue within the ED & inpatient stream: Timely Emergency Care Collaborative – Home (sharepoint.com)
We are proud of…
• Maintaining timely access to care for all of our patients – AV offload within 40 minutes was 75% at FHED in November!
• Ongoing recognition of our staff achievements across the Division
• Paediatric Emergency in-situ and interdisciplinary simulation program
We are looking forward to…
• Reviewing our Sunshine Behavioural Assessment Unit, Hub and Fast-Track models of care with key stakeholders to ensure they are providing Best Care for our patients
• Establishing our new Emergency Medicine Intranet site
• Establishing an ED/HiTH collaboration project
• Sunshine ED refurbishment
• Review of General Internal Medicine model
• EMR implementation at Bacchus Marsh and Melton
• Improving patient access to our EMA outpatient clinics through the use of guidelines and other improvement initiatives
Our focus continues on…
• Addressing our Falls & Pressure Injuries across the Division
• Improved compliance with risk assessments and utilisation of iPOCS across our inpatient areas
• Improving medical and nurse practitioner staffing (particularly across our EDs and Urgent Care Centres)
|
Data Analysis |
Key Message |
||||
|
Hand Hygiene |
Period 2 of National Hand Hygiene Initiative (NHHI) ended in October with a Divisional result of 89.1% (target = 80%). | Don’t forget to replace the end of bed alcohol-based hand rub if empty. If you do not know where to get a new bottle from in the ward or department, please let the nurse in charge know. | |||
|
Medication Errors |
|
Don’t forget the 5 Rights for medication safety |
|||
|
Comprehensive Care—Falls, Pressure Injuries and nutrition |
|
|
|||
|
Mechanical Restraint |
There have been fewer episodes of Mechanical Restraints across the Division in November and we continue to see improved compliance with appropriate care and documentation.
|
Use least restrictive practice, review and remove as soon as possible. Ensure it is documented. |
|||
| Communicating for Safety | There were 10 incidents related to the Communicating for Safety Standard, with six of these being in our Emergency Departments and Urgent Care Centres. | Please visit our Best Care website for more information about Standard 6 | |||
| Blood Management | There were two blood management incidents across our Division in November – one on 2C and one in FHED. | Complete your mandatory training via WeLearn | |||
| Recognising and responding to Acute Deterioration | There were five reported clinical incidents related to Standard 8 in November, four of which were in our EDs and Urgent Care Centres |
See more about Standard 8: Deteriorating Patient |
| Incidents and Complaints |
|
Standard 1 and Standard 2 |
Quality System Sites
Click on the following images to access information about the quality systems that support staff across Western Health to provide, monitor, review and improve Best Care.
Events
To support Western Health’s vision of best care, the Auditing Best Care (ABC) audit is a tool used to monitor our delivery of Best Care and provides us with an opportunity to identify areas for improvement on how we deliver that care.
ABC Audit day will be held across most inpatient areas across Western Health on Tuesday 14th May 2024.
The audit is to be completed at the following locations:
– All inpatient areas at Footscray, Sunshine, Williamstown and Bacchus Marsh Hospitals
– Short Stay Units (SSUs) at Footscray and Sunshine Hospitals