he latest benchmark reports from the Health Roundtable that go up to September 2023 have recently been released, that show how our delivery of Best Care compares to other health services across Australasia.
Let’s look at how we perform in the area of hospital acquired infections. Hospital acquired infections include urinary tract infections, surgical site infection, pneumonia, blood stream infection, central line and peripheral line associated bloodstream infection, multi-resistant organisms, infection associated with prosthetics/implantable devices, gastrointestinal infections and other high impact infections.
Hospital Acquired Infections:
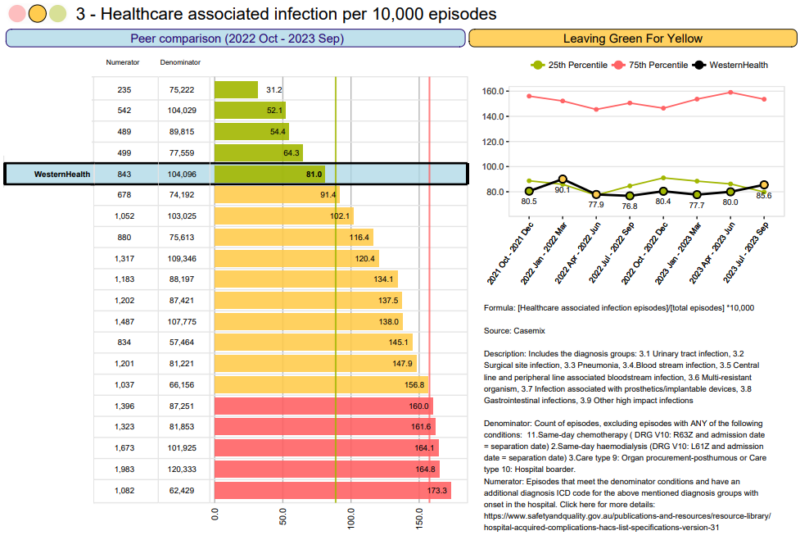
The rates of hospital acquired infections at Western Health has been consistently green but entered into the low amber last quarter.
This means that our patients get far less hospital acquired infections that we do at peer hospitals. This is a wonderful result.
Remember, you can impact these results through:
- Gloves should always be clean: gloves should always be changed between patients, and clean gloves are always required when undertaking any procedure. Hand hygiene is required between changes of gloves, and alcoholic hand rub must never be applied to gloves.
- Hand Hygiene: ensure you undertake the 5 moments of hand hygiene and that there is alcoholic hand rub present at every bed side and point of care.
- Correct skin preparation: whenever an invasive device is being inserted, chlorhexidine skin preparation must be utilised. An alcohol wipe is never an appropriate skin preparation.
- Antiseptic non-touch technique (ANTT): when inserting, accessing, dressing or removing any invasive device, ANTT needs to be utilised. Also please ensure that you use a clean stainless steel dressing trolley, not a kidney dish, bedside table or the patient’s bed.
- Only insert a device if it is needed: Always ‘hesitate before you cannulate’. Does the patient really need that device inserted? Never insert a device ‘just in case’. Any invasive device is a potential source of infection, so let’s minimise them where we can.
- Remove the device as soon as it is not needed: As soon as a device is no longer needed, remove it as quickly as possible. Ask medical staff to change IV orders to oral orders where appropriate. The longer devices are in situ, the greater the risk of an infection occurring.
Carbapenemase-producing organism (CPO) is a collective term that refers to a group of bacteria that have become resistant to many antibiotics, including our last line of defence antibiotics called carbapenems.
including our last line of defence antibiotics called carbapenems.
Along with many other health services, Western Health has seen a rise in CPO cases since January 2024. Currently CPO is in 5 of our wards and unfortunately for the first time in our Western Health history some internal transmission has occurred. This is a notifiable event and our Infectious Diseases and Infection Prevention teams have been working with the Department of Health.
An Incident Management Team has been established to oversee the rapid implementation of short-term measures to decrease the risk of further internal transmission.
In addition, we’re asking all staff to continue adhering to standard infection prevention practices to help us stop the spread,
About CPO
Some people carry CPO in their gut and remain healthy but if the CPO moves from the gut to another part of the body, they may develop an infection and require treatment. The CPO produce an enzyme called carbapenemase that makes the antibiotic no longer effective in fighting infections, resulting in limited treatment options and often death.
CPO infections are rare in Australia and are usually associated with overseas hospital admissions or healthcare, particularly in parts of Europe, North America, the Middle East and Asia. Groups at increased risk of acquiring CPO include:
- people have had prolonged admissions to hospitals
- people who have received medical care or aged care overseas in the previous 12 months
- people who have been treated with multiple or repeated courses of antibiotics
- people with a weakened immune system or underling long-term medical conditions
- people with an indwelling medical device such as a urinary catheter.
What can I do?
Essentially, we just need all of our staff to adhere to standard infection prevention practices. Please be cognisant that every action that you do will impact on whether CPO is contained or spread – depending on how you do it!
Top tips for positively impacting on our ability to contain CPO:
- Screening: Finding CPO on people who carry CPO is essential to stop any spread. This is why we have an infection prevention infectious risk screening questionnaire in our EMR to be done on admission for all our patients – it is essential that this is done as early as possible, preferrably at the entry point (usually Emergency Department, Urgent Care Centres or Day Surgery Units). If someone has a history of being in an overseas hospital, having a procedure or being in a residential care facility in the last 12 months, a specimen to look for CPO (either a stool sample or a rectal swab) must be collected, patient isolated in single room, own bathroom. CPO High Risk alert placed, and Infection Prevention notified.
- Handover: as CPO is relatively new to Australia, there may be some staff that are not aware of what it is, and how serious it is. Please ensure that if a patient has CPO, or is a contact of CPO cases it is included in each handover to ensure that staff make good, informed decisions on how they practice. Check the infectious risk alerts to see why patients are in Contact precautions.
- Isolation: Contact transmission-based precautions are used in addition to standard precautions to prevent the spread of CPO. Contact precautions need to be followed, including wearing gloves and a gown before entering the room of a CPO patient, and taking them off prior to exiting. Patients with CPO are the highest priority for single rooms; however Infectious Diseases and Infection Prevention may approve cohorting of patients with the same strain of CPO.
- No equipment or devices to enter and exit rooms: Shared equipment and devices (including WOWs, vital signs machines, glucometers, and stethoscopes) can be the greatest spreaders of infection across hospitals. Nothing should be routinely entering and exiting rooms being used to isolate a patient with CPO. Western Health has recently moved to using disposable equipment and dedicated devices for use with all patients with CPO. Room computers should be used to avoid contaminated WoWs entering rooms.
- Carefully cleaning and disinfecting rooms: rooms need to be regularly cleaned and disinfected. CPO rooms also get ultra-violet marker testing to validate the cleaning effectiveness. Anything that does need to leave the room needs to be thoroughly cleaned and disinfected. Make sure that simple easy slip-ups don’t occur, like putting contaminated meal-trays on clean PPE trolleys.
- Shared patient equipment: if shared patient equipment must be used, it must be cleaned after each use. Small pieces of equipment must be cleaned using the disinfectant wipes, ensuring all surfaces are cleaned. Large pieces of equipment such as lifting hoists should be cleaned with Actichlor (chlorine based) product with microfibre cloths.
- Hand hygiene:ensure you undertake the 5 moments of hand hygiene and that there is alcoholic hand rub present at every bed side and point of care. Gloves should be removed, hand hygiene performed and gloves redonned when moving from contaminated area to clean area. Hand hygiene must be performed immediately before donning gloves, and immediately after removing gloves. Gloves should always be put on immediately prior to touching the patient in the room or cubicle, not outside the room. Gloves should not be kept on PPE trolley’s but inside the room to avoid cross contamination of gloves. Review Using gloves appropriately in healthcare (vimeo.com)
- Careful staff allocation: where possible, try to allocate staff that are caring for patient(s) with CPO so that they are not caring for patients without CPO to decrease the risk of transmission.
- Antimicrobial stewardship: This is the range of activities that reduces the unnecessary and inappropriate use of antibiotics to prevent and contain antimicrobial resistance. Antibiotics should only be dispensed and administered if they have the necessary approvals from our Infectious Diseases clinicians.
- Patient hand hygiene: patients will have hand wipes added to their meal trays to encourage hand hygiene prior to eating, to avoid oral ingestion of organisms from their environment. Please encourage patients to use the wipes before eating. Also remind patients to wash their hands after using the bathroom and to use the hand rubs if they ambulate around the ward or go out to the café’s on exiting and returning to their room.
Thanks to everyone who submitted projects for consideration for Best Care Awards, the competition for the awards was exceptionally high with the judges commenting on the high quality and diverse nature of the submissions.
Congratulations to all those who were successful:
SAFE CARE AWARD
Project LINEZ: A Quality Improvement project aimed at reducing CLABSI to zero in newborn services
Summer Chambers, Mei Lee, Spania Khun and Kate Law – New Born Services
Having identified that our New born Central Line Associated Bacterial Infection was approximately twice the National average the team took action. Firstly looking at the processes involved and areas of high risk the team drew up procedures to minimise the risk as part of their safety bundle. This was implemented with their team and coupled with vigilance and monitoring.

PERSON CENTRED CARE AWARD
ERAS – Enhanced Recovery After Surgery
Rebecca Fewster, Phong Tran, Claire Burrows, Raheela Datoo, Chris Weiers, Mary De Gory, Mathhew Thorpe, Abi Davis, Rachel Kropman, Richard Grygiel
ERAS priorities person-centred care, by tailoring surgical optimization by ensuring that patients are helped across all aspects of care prior to surgery. Through the tailoring of the care provided for hip and knee replacement the ERAS team has been able to reduce the length of stay in hospital by 1.5 days on average, while reducing readmission rates. Delivering safe and patient centred care.

COORDINATED CARE AWARD
Footscray Short Stay Unit Flow
Ainslee Senz, Elizabeth Borowik, Renie Lloyd, Doriana Andreou – Footscray Emergency Department.
The Short Stay Unit is crucial in achieving the flow required to see new patients in a timely manner. The team identified two interventions to implement in the unit – capping the number of patients admitted to the SSU and allowing better flow by defining criteria for direct admission. By implementing these changes the unit was able to see measurable improvement in the way the SSU ran but also the whole of the ED.

RIGHT CARE AWARD
Improving Outcomes for Acute Inpatient Orthopaedic Patients
Sarah Saxionis, Chelsea Baxter – Occupational Therapy
In this project it was identified that patients regularly had to wait 24-72 hours for equipment delivery to ensure that they were able to return safely home. Time that was delaying discharge. Using the IHI model for Improvement Sarah and Chelsea were able to implement a number of small PDSA cycles to ensure Right OT equipment was available to the consumer when needed. As a consequence the patient can go home sooner.

BEST CARE IMPROVEMENT IDEA AWARD
Improving Communication Handover and Teamwork (iCHAT) in New Born Services
Kate Law, R Lim, M Ryan, N Brotonel, J Whitelaw, N Toumbourou, J Padre, G Foo, A Sett
Prioritising the care of critically unwell infants admitted to Newborn Services (NBS) is of paramount importance. These fragile infants demand the expertise of highly specialized and skilled staff equipped with a broad spectrum of knowledge and abilities. Advanced communication techniques are required to impart vital information in complex healthcare settings such as NBS and can pose a significant risk to patient safety if inadequately delivered. Optimising systems of communication and handover play an instrumental role in reducing errors, by facilitating the accurate and efficient transfer of information amongst all members of the multidisciplinary care team. The benefits of an optimised handover format and communication culture align with Western Health’s strategic vision for prioritising patient outcomes, safety and wellbeing.

Once again thankyou to everyone who submitted, the BCGS team for organising the awards and the judges for their time.
All projects submitted for the awards are available in the Improvement Project Showcase on the Improvement Tab of the Live Best Care Site.
Hospitals rely heavily on portable medical equipment, with workstations on wheels (WOWs) being among the most frequently used devices. Consequently, these carts can serve as potential sources of infections if proper precautions are not taken during their use and maintenance.
Maintain a Clutter-Free Environment
Medical carts can quickly become pretty messy if users are not vigilant. It is crucial to ensure that clutter is kept off the WOWs to prevent the risk of infections. It is important to remember that WOWs are not intended for use as procedure trolleys. By keeping them clutter-free, we reduce the surface area available for bacteria and other pathogens to thrive.
Regular Cleaning and Disinfection
Given the pivotal role that WOWs play in our healthcare facilities, they also present a risk of transmitting infections among patients and staff. These machines are susceptible to contamination from the hands of healthcare workers (HCWs). Numerous studies have revealed that both pathogenic and non-pathogenic organisms can persist on WOW surfaces for extended periods. Therefore, it is imperative for healthcare workers to understand the significance of cleaning and disinfecting WOWs. Here are some guidelines for maintaining cleanliness:
- Wipe Down at the Start of Each Shift: The WOW should be wiped down at the beginning of every shift.
- Clean Before Changing Locations: Clean the WOW before moving it to another bed space or patient room.
- Use a Neutral Detergent Wipe: Utilize a neutral detergent wipe that is available on the WOW for cleaning.
- No Personal Belongings: Do not place staff belongings, staff beverages, water bottles, meal trays, or linen on the WOW.
- Gloves Off for Computer Use: Do not wear gloves when operating the WOW computer or computer device.
- Prioritize Hand Hygiene: Perform hand hygiene before and after touching the WOW.
- Hand Hygiene Protocol: Adhere to hand hygiene protocols following interactions with the computer device and before touching the patient (Moment 1).
Managing Patients with Transmission-Based Precautions
In cases where patients require transmission-based precautions (such as respiratory and contact precautions), it is crucial to follow specific guidelines:
- No WOWs in Patient Rooms: WOWs must not be taken into the rooms of patients with transmission-based precautions.
- Avoid Device Use in Patient Rooms: Staff should refrain from using the device in the rooms of patients with transmission-based precautions.
- Proper PPE Removal and Hand Hygiene: Staff should remove all personal protective equipment (PPE) and perform hand hygiene before touching the WOW outside the patients’ room.
By diligently adhering to these guidelines, we can reduce the risk of infections associated with WOWs and ensure the safety of both patients and healthcare workers.
Staphylococcus aureus is the most frequently isolated bacterial pathogen in wounds. Staphylococcus aureus is an important cause of both acute and chronic wound infections. Many of our patients present to hospital with pre-existing wounds. Almost all wounds are colonized with a spectrum of microbes. However, only some of them are considered infected wounds. Western Health has seen several recent Staphylococcus aureus bacteraemia (SAB) that were wound related but not swabbed on admission and then deemed healthcare acquired because the blood stream infection was detected more than 48 hours after admission. If swabbed early in admission then these SABs would be deemed community acquired and not Western Health acquired.
and chronic wound infections. Many of our patients present to hospital with pre-existing wounds. Almost all wounds are colonized with a spectrum of microbes. However, only some of them are considered infected wounds. Western Health has seen several recent Staphylococcus aureus bacteraemia (SAB) that were wound related but not swabbed on admission and then deemed healthcare acquired because the blood stream infection was detected more than 48 hours after admission. If swabbed early in admission then these SABs would be deemed community acquired and not Western Health acquired.
Do your patients wound need swabbing within 48 hours of admission?
Part of our initial assessment of a wound is to determine whether a wound swab is required. A wound should only be swabbed if there are clinical signs of infection and the wound is deteriorating, increasing in size or failing to heal.
The classic clinical signs of infection in an acute wound include:
- New or increased pain
- Swelling
- Erythema
- Purulent exudate/discharge (or serous exudate with inflammation) There is often purulent discharge and, depending on the offending organism, may have a strong odour.
- Malodour or unpleasant smell
- Localised warmth around the site of the wound
Signs of spread of a localised wound infection include extension of erythema (and development of cellulitis), abscess formation, lymphangitis, crepitus in the soft tissues and breakdown or dehiscence (splitting open) of the wound.
If your initial nursing assessment includes any of the above your wound needs to be swabbed within 48 hrs of admission for a multitude of reasons
- A swab can shed light on the potential complications in wound care if there is a microorganism present such as Staphylococcus aureus
- For local wound evaluation, wound swabs can be valuable for surveillance of the flora colonising a wound
- Assists with the treatment plan
- Assists with optimal wound management and antibiotic usage based on the assess
It is imperative we incorporate our patient’s voice in everything we do. Person-centred care is globally recognised as the gold standard approach to healthcare delivery. Partnering with patients in their own care has never been more important from an infection prevention perspective for their best health outcomes.
Peripheral Intravenous Catheter (PIVC) associated Staphylococcus aureus Bacteraemia (SAB) infections account for close to 40% of all hospital acquired SAB infections. 25% of hospitalised patients die post contracting a SAB infection. This is just one organism, as PIVC related infections from other organisms also has a significant impact on patient safety and patient outcomes. Data from Australia and internationally, overwhelmingly suggest that a large proportion of patients with a PIVC do not receive the recommended evidence-based care and that such infections are preventable.
In a show of commitment to reducing PIVC related SAB’s, Western Health’s SAB Taskforce has created a patient centred approach to PIVC care by providing health information in engaging and accessible formats like our cannula care consumer screen saver and poster. We encourage all areas to display the cannula care screen saver on TV screens at ward entrances to engage with our consumers to drive and sustain service improvement.
Click on the following to access the image:
Western Health has continued to closely monitor the status of COVID in our facilities and across the community. This information has informed our COVID settings which have periodically escalated and de-escalated based on the level of risk.
Unfortunately, COVID will continue to remain a factor that we need to take into consideration to provide a safe environment for our staff, patients, volunteers and the public.
Based on our experience and evidence, Western Health is now moving to a COVID Sustainability matrix to inform our settings from this point forward. The matrix is outlined below and aims to provide a transparent and simplified guidance for our staff and volunteers, and includes the trigger points that we will use to inform our settings.
The matrix provides guidance on:
- masking and visitor guidance based on whether the health service is red or green:
- how settings change in wards/departments where there is a patient(s) with COVID or suspected COVID (SCOVID); and
- the definition of an outbreak ward, and control measures to be implemented if a ward/department meets this definition.
In accordance with the matrix below, Western Health’s COVID status is currently Green, therefore the relevant masking and visitor settings can be put in place in your area as outlined below. If a ward/department has patients with COVID or SCOVID or meets the definition of an outbreak ward, please continue to wear a P2/N95 respirator whilst in that environment.

We will continue to monitor the data and will formally advise all staff and volunteers any change to our status in the future.
We continue to be committed to providing a safe environment for all of our staff, patients, volunteers and visitors and again thank you for your commitment and support.
With WH being one of the most impacted organisations in Victoria and nationally during each wave of the COVID-19 pandemic significant infection prevention resources were implemented.
Two Infection Preventionists were seconded into the COVID preparedness team for 6 months to prepare the organisation, and a standard and transmission-based precautions (S&TBP) online module was developed for all staff. A dedicated Coronavirus microsite was developed as the source of truth which was accessible externally and readily accessible with frequently changing communications and guidance.
 A PPE Champion program was initially developed to foster a ‘Buddy’ PPE system to keep each of the clinical staff safe which was overseen by one of the COVID Response team members with IP input for education. A PPE Spotter program was subsequently implemented with training provided over Zoom and then moved to an online training module. Shift PPE Spotter reports were initiated to ensure safe practice and to act on any identified issues or gaps for training. Significant PPE breach issues were actioned by the PPE Spotter Coordinator in IP with escalation as required.
A PPE Champion program was initially developed to foster a ‘Buddy’ PPE system to keep each of the clinical staff safe which was overseen by one of the COVID Response team members with IP input for education. A PPE Spotter program was subsequently implemented with training provided over Zoom and then moved to an online training module. Shift PPE Spotter reports were initiated to ensure safe practice and to act on any identified issues or gaps for training. Significant PPE breach issues were actioned by the PPE Spotter Coordinator in IP with escalation as required.
Quick Reference Guidelines, posters, training videos, communications were regularly reviewed and updated on the Coronavirus microsite with each Victorian guidance changes by IP and the COVID Response team. IP representation was included in the PPE Core Working group and the PPE Clinical Taskforce who oversaw the WH PPE Guidelines and communicated all changes. Victorian COVID Safe workplace plans were undertaken as required and submitted to DH and located on the microsite. WorkSafe Victoria would also undertake local audits with the OH&S team as required.
IP engagement was sought when setting up or expanding testing sites in the community or internally as well as input into one of 3 Metro Vaccine Hubs set up out of Sunshine Hospital for COVID vaccination programs for staff and the community. Community outreach vaccination programs were also set up to support vaccinations in high-risk areas in the community with a large proportion of migrant representation from non-English speaking backgrounds as well as RACF’s.
A dedicated Contact Tracing (CT) team was established in mid-2020 led by one of the IP team members who oversaw all internal patient and staff contact tracing with the Western Public Health Unit (WPHU) responsible for all community management and response. The CT team progressively expanded with subsequent waves and oversaw all outbreak management in conjunction with IP and ID, they reviewed all healthcare worker infections with use of automated RedCap surveys for staff and utilisation of MS Teams to support contact tracing by all team members including remotely and outbreak management.
 Utilisation of the locally invented McMonty Ventilation Hood greatly supported the reduction in the number of HAI infections to other patients with a fleet of ~191 hoods in use across the organisation as did significant investment in air purifiers in clinical areas and break rooms. This was done in conjunction with air handling audits to identify problem areas and boost air exchanges per hour in all patient areas plus air directionality reviews by Melbourne University Engineering Department.
Utilisation of the locally invented McMonty Ventilation Hood greatly supported the reduction in the number of HAI infections to other patients with a fleet of ~191 hoods in use across the organisation as did significant investment in air purifiers in clinical areas and break rooms. This was done in conjunction with air handling audits to identify problem areas and boost air exchanges per hour in all patient areas plus air directionality reviews by Melbourne University Engineering Department.
A dedicated team of medical staff (Deisolation Team) undertook the clinical side of COVID response management 24/7 by reviewing all results, communicating them to clinical areas in real time of results becoming available, following up on newly identified staff cases with test results, approving rapid PCR testing in conjunction with IP CNC’s, developing testing criteria, risk categorisation, de-isolation and bed allocation guidelines and communicating to treating teams plus having oversight on deisolating of all SCOVID and COVID patients. Regular meetings are held several times per week to discuss outbreaks, issues across sites and for planning purposes between CT team, IP, Infectious Diseases, Desiolation team and the DON for Standard 3.
 Infection Prevention supported the WPHU IP persons to go out to outbreak community RACF’s to undertake reviews, provide support and report back to the aged care sector of DH.
Infection Prevention supported the WPHU IP persons to go out to outbreak community RACF’s to undertake reviews, provide support and report back to the aged care sector of DH.
Footscray Hospital participated in a VICNISS pilot program for additional dataset with community and hospital administered antiviral treatment and morbidity datasets to support the Victorian Chief Health Officer identify potential gaps in timeliness for antivirals which was subsequently rolled out to all Victorian hospitals by VICNISS and targeted communication to GP’s.
The Operations Manager of Infection Prevention participated as guest speaker in 2 Safer Care Victoria forums around COVID and PPE given WH’s experience as well as speaking at VICNISS forums about the Footscray hospital pilot for antivirals and morbidity data addition to COVID patient monitoring requirements.

