Published on 1 August 2023
Edition 70: August 2023
-
Helpful contacts
Employee Assistance Program: 1800 099 444
Nurse & Midwife Support: 1800 667 877
Nurse & Midwife Health Program: 03 9415 7551 or 1800 888 236
-
Upcoming dates
August 2023
1 Riskman upgrade
3 Unit Manager Breakfast Meeting
4 Aboriginal nurse and midwife post-graduate scholarship closes
7 Aged Care Employee Day
7 National Stroke Week
8 Nursing & Midwifery Open Forum (2pm)
9 National Nursing Forum (Australian College of Nursing) commences in Adelaide
14 SCV Health Innovators Program EOI deadline
15 Deadline for mandatory flu vaccination for all Category A and B healthcare workers
16 Catch up with Russell webinar (2pm)
29 Let’s Talk Leadership (Australian College of Nursing)Check out Events for more details.
-
Nursing & Midwifery Executive
Adjunct Professor Shane Crowe
Executive Director of Nursing & Midwifery
Phone: 8345 1463
Email: shane.crowe@wh.org.auProfessor Bodil Rasmussen
Chair of Nursing, Deakin University/Western Health
Phone: 8395 8163
Email: bodil.rasmussen@wh.org.auDoug Mill
Director of Nursing & Midwifery
Division: Chronic & Complex Care
Phone: 0400 807 938
Email: douglas.mill@wh.orh.auHelen Sinnott
Director of Nursing & Midwifery, Sunshine
Phone: 0435 962 716
Email: helen.sinnott@wh.org.auAdjunct Associate Professor Jo Mapes
Director of Nursing & Midwifery, Footscray
Division: Perioperative and Critical Care
Phone: 0423 302 337
Email: joanne.mapes@wh.org.auKylee Ross
Acting Director of Nursing & Midwifery Informatics (CNMIO)
Phone: 0409 555 384
Email: kylee.ross@wh.org.auLena Pejcinovski
Director of Nursing, DPFC
Division: Custodial Health
Phone: 0422 818 187
Email: lena.pejcinovski@wh.org.auProfessor Linda Sweet
Chair of Midwifery, Deakin University/Western Health
Phone: 8395 1178
Email: linda.sweet@wh.org.auLisa Gatzonis
Director of Nursing & Midwifery Workforce
Phone: 9393 0127
Email: lisa.gatzonis@wh.org.auMonique Sammut
Director of Nursing & Midwifery, Sunbury
Divisions: WPHU and Clinical Support & Specialist Clinics
Phone: 0412 769 423
Email: monique.sammut@wh.org.auNicole Davies
Director of Nursing & Midwifery, Williamstown
Division: Emergency, Medicine & Access
Phone: 0435 656 190
Email: nicole.davies@wh.org.auRobyn Peel
Director of Education & Learning
Phone: 0468 608 141
Email: robyn.peel@wh.org.auRohan Vaughan
Director of Nursing & Midwifery, Melton
Division: Drug Health
Phone: 0434 365 769
Email: rohan.vaughan@wh.org.auRyan Dube
Director of Nursing
Senior Mental Health Clinical Lead
Division: Mental Health & Wellbeing
Phone: 0420 228 035
Email: ryan.dube@wh.org.auAdjunct Professor Tanya Farrell
Director of Maternity Services
Division: Women’s & Children’s
Phone: 0468 830 755
Email: tanya.farrell@wh.org.auVal Dibella
Acting Director of Nursing & Midwifery (Inspiring Innovation)
Phone: 0466 489 687
Email: val.dibella@wh.org.auWendy Giddings
Director of Nursing & Midwifery, Bacchus Marsh
Divisions: Aged, Cancer & Continuing Care and Bacchus Marsh & Melton
Phone: 0458 603 897
Email: wendy.giddings@wh.org.au
From Shane

July was a huge month at Western Health, with Stage 2.1 of the EMR successfully implemented and our new colleagues in the Mental Health & Wellbeing Division and at Dame Phyllis Frost Centre settling in to being part of the Western Health team.
These 3 changes are significant transformational reforms, which take a huge amount of hard work and dedication from everyone involved. My sincere thanks to you for the role that you have played in making these changes successful, and for your continued commitment to the provision of Best Care to our community.
During July I was also incredibly proud to be part of the team from Western Health sharing our success, learning, methodology and tools with the rest of the healthcare sector and beyond to decrease occupational violence and aggression. We have fantastic people here at Western Health – this was on show, palpable and it was remarkable!
I remain very focused on our nursing and midwifery workforce, as workforce shortages continue to be a significant threat across the health sector both now and into the future. The good news is that we are in a remarkably good position – and this has not happened by accident!
Despite our growth and it being the middle of winter, our vacancy rate for nursing and midwifery is currently 2.58% (52 EFT) which is incredibly low (it was 4.79% at the same time last year). At the moment we have:
- 265 graduate nurses and midwives in their first year. We have received over 700 applications for our graduate program next year. This is an increase on last year, which is great!
- 29 Enrolled Nurse early career program participants.
- 180 nurses and midwives undertaking post-graduate study. We have increased the number of nurses with specialist post-graduate skills and education by 300% over the past few years.
- decreased our attrition rate from 7.3% to 6.5%. This means that less nurses and midwives are leaving Western Health.
We are in a good position due to us taking a strategic and planned approach at Western Health through the implementation of the actions from our Nursing & Midwifery Workforce Plan 2022-26. Over the past 12 months we have:
- Developed and implemented an international and national recruitment relocation package.
- Evaluated, enhanced and embedded the RUSON and RUSOM programs.
- Increase in undergraduate student placement opportunities.
- Implemented a Transition to Acute Care program.
- Implemented actions to improve recruitment experience for candidate and managers.
- Expanded graduate employment models.
- Worked with universities to commence enhancing our secondary school relationships and explore pathways and employment models.
- Reviewed, updated and clarified Clinical Nurse Specialist / Clinical Midwife Specialist application process, including for Mental Health & Wellbeing.
- Significantly increased post graduate scholarships offered, across all areas including ED, ICU and an increased number of other specialties.
- Expanded clinical assessment learning opportunities, through the new Patient Assessment Program.
- Launched Lippincott to improve access to quality care provision resources.
- Launched the first tranche of meaningful Data Dashboards for all stakeholders.
A significant initiative coming out of our Workforce Plan is the Employee-centered Rostering Project, which aims to enhance retention and employee engagement through the use a co-design approach to increase the flexibility, transparency and satisfaction with nurse and midwife rostering. We are entering into the co-design phase of this project, so I encourage you to get actively involved!
Finally, the new Mental Health & Wellbeing Act will commence on 1 September 2024. I have provided more information below for our mental health and wellbeing nurses in the lead up to this legislative change.
Shane Crowe
Executive Director, Nursing & Midwifery
No more on the floor

Despite our best efforts, many dangerous germs lurk in hospitals. So how dirty are hospital floors?
According to an emerging body of research hospital floors are very dirty. A recent study found that floors in patient rooms were often contaminated with MRSA, VRE, and C. diff. The most frequently found pathogen was C. diff – in both the C. diff isolation rooms and non-C. diff isolation rooms. The results were very similar amongst each of the 5 hospitals in the study. The results are pretty disconcerting because the pathogens found can lead to hospital-acquired infections.
Even if people don’t directly touch the floors, other things that patients, visitors, and staff routinely touch are in contact with the floor. Unfortunately, it is not uncommon for high-touch objects such as medical devices, personal items, and linens to be in direct contact with the floor and demonstrates the potential for indirect transfer of pathogens to hands from fomites placed on the floor.
This is a timely reminder that hospital floors are an under-appreciated source for dissemination of pathogens and can be spread quite easily if we don’t minimise interactions with our floors.
There is a lot we can do to help reduce the risk of getting an infection from the pathogens on hospital floors like:
- not letting linen touch the floor,
- blow up air mattresses on a bed and never on the floor,
- keep indwelling catheter bags off the floor,
- always perform the 5 moments of hand hygiene and
- remember no more on the floor.
The month of August will see infection prevent and CEL relaunch the No More on the Floor campaign and looking forward to your support.
Employee-centered Rostering Project update

Rostering is an important process to enable efficient, effective and safe delivery of health care. However, shift work has been shown to be associated with several negative health outcomes for nurses and midwives including burnout, fatigue, headaches, social isolation, mental distress and sleep disorders. In particular, night shifts, early morning shifts, quick returns and requests to work on scheduled days off are known to cause significant sleep loss and contribute to fatigue. Nurses’ quality of professional life has also been shown to be significantly affected by shift duration, time and frequency.
As well as the negative health-related outcomes, shift work may also influence nurses’ and midwives’ career-related decisions including their intention to remain in their job or in the professions. Intention to leave an employer or the professions tends to be higher among nurses and midwives who are less satisfied with their jobs, experience conflict managing their paid work and family responsibilities, work night shifts or rotating shifts. Experienced nurses have identified that a lack of flexibility in their work schedules as an important factor in their decisions about retiring.
There is evidence to suggest that more flexible working/shift patterns and self-rostering/scheduling systems can improve nurses’ and midwives’ work-life balance, health and wellbeing, job satisfaction and retention.
Western Health is undertaking this important project using a co-design approach to identify the rostering concerns, needs and preferences of nurses and midwives. Based on the findings we want to implement and evaluate co-designed acceptable, equitable, transparent and feasible rostering guidelines.
Where are we up to?
Our nurses and midwives have now completed pre-implementation survey and participated in a pre-implementation focus group. The next phase is co-design.
Co-design process:
Western Health is committed to co-designing the way rostering will work in the future with our nurses and mdiwives.
All nurses and midwives will be invited to participate in a co-design workshop. Two workshops will be held – one for nurses and one for midwives using WhatsApp. The use of WhatsApp as the platform for the co-design workshops enables participation at times that suit participants. It is easy to access via personal computers, smartphones and tablets, removing the need for a physical venue, and is a space in which people are comfortable and open to discussing their ideas and opinions. WhatsApp is a highly secure messaging app which uses end-to-end encryption on all chats.
Nurses and midwives who are interested in participating in the study will be invited to join the study’s WhatsApp group. There will be guidelines about participating in the group such as respecting the privacy of other group members, not disclosing or sharing comments posted as part of the group discussion with those outside group and treating other members of the group with respect.
Participants will also be asked to undertake a demographic survey outside of WhatsApp.
Data from the pre-implementation survey and focus groups will be used by the research team to draft revised roster guidelines. The co-design workshops will discuss and evaluate the revised roster guidelines in terms of their comprehensibility, salience, and acceptability for nurses and midwives and refine the guidelines based on the findings. A discussion guide will be used to prompt and initiate discussion about the revised guidelines and whether changes are required before they can be used at Western Health.
Western Health leading the way with preventing OVA

There was a fantastic energy and engagement in the room during Western Health’s Occupational Violence and Aggression Conference in July.
We were joined by colleagues from across the health sector and government as well as representatives from other industries at higher risk of OVA to share our Predict, Prevent, Priority: Safety package and learning.
Highlights included keynote addresses from the Health Report’s Dr Norman Swan, Victoria Police’s Assistant Commissioner Luke Cornelius and futurist Alex Hagan as well as insights from Western Health staff who drove and championed our OVA program.
We also hosted panel discussions and practical sessions where we explored case studies, looked at impactful tools and training, and learned from the real-world experiences of our frontline workers.

MC Karen Percy in wrapping up the event had this to say: “OVA is too big to ignore. It’s critical in the healthcare sector but there are some universal issues across many sectors. We know there are solutions out there. It takes leadership and a shift in attitude to put one’s safety first. It takes mandatory changes in your practice and to evolve as needed.
“Today, we’ve heard statistics of how effective these changes have been at Western Health – fewer injuries, incidents handled in a controlled and planned way, and staff feeling supported. Change isn’t going to happen overnight but change is possible. When staff are safe, there are better outcomes for patients, organisations and for the staff themselves.”
Thank you to all our keynote speakers, presenters, MC Karen Percy, Uncle Tony Garvey for his Welcome to Country, and conference participants.
New Mental Health & Wellbeing Act commencing soon

The new Mental Health and Wellbeing Act 2022 (the Act) will commence 1 September 2023. On 17 July 2024 the Department of Health released a fact sheet on frequently asked questions regarding the new Act.
Foundations for a new mental health system:
The new Act resets the legislative foundations of Victoria’s mental health and wellbeing system. It establishes key entities in the new system architecture and includes broader regulation to support a safer, more inclusive system. The definition of Mental Health and Wellbeing Service Provider includes a wider range of service providers.
Support and education:
Western Health has an Implementation Lead employed, who is working closely with the Department of Health to develop consistent education packages for the new Act. These packages are expected to be implemented throughout August.
Additionally, the Department of Health is developing a series of e-learning modules to introduce the workforce to the new Act. This includes key changes from the Mental Health Act 2014. The introduction of training modules will be phased over time and include topics such as the new rights-based principles, protection of consumer and carer rights, and the role of key oversight bodies.
More information:
Some of the major changes in the new Act (found on the Department’s website) are summarised below:
-
Aboriginal Social and Emotional Wellbeing:
The Act includes a Statement of Recognition of Aboriginal people and acknowledgement of the Treaty process. The Statement enshrines commitments to Aboriginal self-determination in Victorian Government health statutes for the first time. A key objective of the Act is the provision of culturally safe and responsive services to Aboriginal and Torres Strait Islander people to support and strengthen connection to culture, family, community and Country.
The cultural safety principle requires mental health and wellbeing service providers to provide culturally safe and responsive mental health and wellbeing treatment and care to Aboriginal and Torres Strait Islander peoples that is appropriate to, and consistent with, their cultural and spiritual beliefs and practices.
The information sharing principles set expectations that the health and personal information of Aboriginal and Torres Strait Islander peoples is to be treated in a way that is culturally safe, promotes self-determination and acknowledges connections to family, kin and community.
-
Rights-based objectives and principles:
New objectives aim to achieve the highest attainable standard of mental health and wellbeing for Victorians. New rights-based mental health principles prioritise the values, preferences and views of consumers, families, carers and supporters. Principles support the Royal Commission’s ambition of reducing the use of compulsory treatment and restrictive interventions.
The Act sets a higher standard of accountability to embed the principles into daily practice. For the first time, mental health legislation includes a diversity of care principle, a least restrictive care principle and a principle to support the health, wellbeing and autonomy of children and young people.
Mental Health and Wellbeing Providers must give proper consideration to the principles when making decisions and must make all reasonable efforts to comply with the principles when exercising a function under the Act. Complaints can be made to the new Mental Health and Wellbeing Commission if a service provider fails to comply with these obligations. Mental health and wellbeing service providers are required to report on how they are responding to the mental health principles in annual reports.
-
Lived experience:
The new Act puts people with lived and living experience of mental illness and psychological distress, and their families, carers and supporters at the centre of the mental health and wellbeing system. It does this through the inclusion of new rights-based objectives and principles and designated lived experience roles at the highest levels of new and existing governance and oversight entities. This includes designated lived experience Commissioner roles within the new Mental Health and Wellbeing Commission and various Boards.
The lived experience principle recognises the importance and value of the contribution of people with lived experience as leaders and partners in the mental health and wellbeing system.
-
Supporting individuals:
New measures promote supported decision making and the agency and autonomy of people living with mental illness. This includes the provision of appropriate supports to help people understand information, communicate and make decisions. All reasonable efforts must be made to provide supports any time the Act requires communication with a consumer or their family members, carers and supporters.
Advance statements of preference (formerly advance statement) may now include a broader range of preferences relating to treatment, care and support needs.
Designated mental health services are now obliged to make all reasonable efforts to give effect to a patient’s advance statement of preferences and/or to support a nominated support person. Written reasons must now be provided whenever a treatment preference outlined in an advance statement of preference is overridden.
The Act clarifies the role of the nominated support person (formerly nominated person) to focus on advocating for the views and preferences of the patient and supporting them to communicate and make their own decisions.
Provisions related to second psychiatric opinions are comparable to those of the Mental Health Act 2014, except for a new requirement that a patient is automatically provided with written reasons when recommendations of a second psychiatric opinion are not adopted. The Act establishes a new opt out model of non-legal mental health advocacy. Service providers must assist mental health advocates in undertaking their role.
-
Treatment and care:
Compulsory assessment criteria and compulsory treatment criteria are unchanged from the Mental Health Act 2014. An independent review of compulsory treatment criteria and the alignment of decision making laws will make recommendations to government to inform future amending legislation.
Provisions related to the use of restrictive interventions are comparable to those of the Mental Health Act 2014, however with the addition of:
- obligation on providers to aim to reduce the use of restrictive interventions with the eventual aim of eliminating their use
- requirements to document alternatives tried or considered
- obligation to review the use of restrictive interventions and to offer an opportunity for the person subject to these interventions an opportunity to participate in the review.
Provisions for the making, variation and revocation and operation of assessment orders, court assessment orders, temporary treatment orders and treatment orders are comparable to those of the Mental Health Act 2014, however, new decision making principles for treatment and interventions must be given proper consideration in the application for and making of these orders.
The Act introduces regulation of chemical restraint as a type of restrictive intervention. Chemical restraint is defined as the giving of a drug to a person for the primary purpose of controlling the person’s behaviour by restricting their freedom of movement but does not include the giving of a drug to a person for the purpose of treatment or medical treatment.
Provisions related to treatment, medical treatment and neurosurgery are comparable to those of the Mental Health Act 2014. The maximum duration of a community treatment orders has been reduced from 12 months to 6 months.
Provisions related to Electroconvulsive treatment (ECT) are comparable to those of the Mental Health Act 2014, although with some drafting changes to clarify the provisions.
Provisions related to the presumption of capacity and informed consent are comparable to those of the Mental Health Act 2014.
-
New roles and entities:
The Act establishes new roles and entities including:
- The Chief Officer for Mental Health and Wellbeing (reporting to the Secretary of the Department of Health with role and functions similar to the Secretary)
- Regional Mental Health and Wellbeing Boards to provide advice to the Minister on the commissioning of mental health and wellbeing services in their regions
- State-wide and Regional Multiagency Panels to bring together service providers and support collaboration and accountability for those requiring ongoing intensive, treatment care and support from multiple services
- A Mental Health Workforce Safety and Wellbeing Committee to provide advice to the Department on the prevention of risks to health, safety and wellbeing of the workforce and approaches to monitoring and responding to these risks.
- Mental Health and Wellbeing Commission: The Act establishes Victoria’s new Mental Health and Wellbeing Commission. The independent statutory authority commences on 1 September 2023. It will play a key role in system-wide oversight of quality and safety and monitor the achievement of the Royal Commission’s goals. The Commission has designated roles for Commissioners with lived or living experience of mental illness or psychological distress and with experience as a family member, carer or supporter. The new Commission will incorporate the existing complaints function of the Mental Health Complaints Commissioner and have a suite of broader powers, including an ‘own motion’ investigation power. Changes under the new Act:
- allow complaints from families, carers and supporters in relation to their experiences in these roles
- align processes and powers with those available to the Health Complaints Commissioners under the Health Complaints Act 2016
- allow for complaints about a failure to comply with obligations in relation to principles.
- Youth Mental Health and Wellbeing Victoria: Youth Mental Health and Wellbeing Victoria (YMHWV) is established as a new entity to:
- provide system leadership and strategic advice, giving agency to the voices of young people with lived experience in response to a crisis in youth mental health; and
- enable a flexible model of delivery and oversight for integrated mental health and wellbeing services for young people by declared operators in specific areas.
- Chief Psychiatrist: The role, functions and powers of the Chief Psychiatrist are comparable to that under the Mental Health Act 2014 however:
- the Chief Psychiatrist’s jurisdiction is defined to include designated mental health services; mental health and wellbeing service providers that provide mental health and wellbeing services in custodial settings; and any other prescribed entity or class of entity
- the new Act no longer provides for separate clinical practice audits by the Chief Psychiatrist. Instead, the clinical review power will have broader application, covering what would have been subject of a clinical practice audit under the Mental Health Act 2014.
- a new role to oversight the use of chemical restraint.
Provisions related to the appointment of Authorised Psychiatrists and delegation of Authorised Psychiatrist powers are comparable to those of the Mental Health Act 2014.
- Mental Health Tribunal: The Act continues the functions of the Mental Health Tribunal which include:
- determining whether the criteria for compulsory mental health treatment as set out in the Act apply and making orders if the criteria are met
- hearing applications for revocation of orders
- hearing and determining applications for certain mental health treatments, including ECT and neurosurgery.
The provisions regarding the Mental Health Tribunal are comparable to those of the Mental Health Act 2014 with minor changes to allow for single member divisions for unopposed adjournment hearings and leave to withdraw proceedings applications.
-
Information sharing:
New principles clarify the purpose and expectations in relation to information sharing. The new provisions in relation to information sharing:
- reflect the new service system by allowing information sharing with specified emergency service providers in an emergency
- specify who can access information from the current electronic health information system and the scope of such access
- enable a consumer to contribute a statement on their health information where a request to correct information has been made under the Freedom of Information Act 1982 or the relevant Health Privacy Principle and the provider has refused to make the correction
- oblige mental health and wellbeing service providers to share information with family, carers or supporters at defined points of care (such as admission or discharge) when a consumer has consented to this disclosure.
Under the new Act information must not be disclosed if there is a risk that a person may be subject to family violence or other serious harm. In other respects, provisions regarding the collection, use and disclosure of information are comparable to those of the Mental Health Act 2014.
-
Health-led response to mental health crises:
New provisions introduced to establish the foundations of a health led response to mental health crises, include:
- new principles that specify powers must be led by a health professional and used in the least restrictive way possible so far as is reasonably practicable
- updated language to reflect a health led approach to mental health emergency
- a capacity to increase the role of health professionals in responding to mental health crises in the community
- new discretions to allow for transfer of care and control between authorised persons and release of a person from care
Recognising the Grant Lodge team on Aged Care Employee Day

Aged Care Employee Day is a National Day of Significance for Australia’s aged and community care workforce held on 7 August each year.
A huge shout out to the amazing team at Grant Lodge and wishing them all a very happy Aged Care Employee Day! Thank you for everything that you do to deliver Best Care to our residents.
The day celebrates the more than 427,000 residential care, home care and retirement living staff who care for over 1.5 million older Australians.
The #ThanksforCaring campaign recognises all the varied roles involved the aged care workforce – from nurses to health care workers, allied health professionals to lifestyle coordinators, volunteers, hospitality teams, drivers, cooks, cleaners, administration staff and so many more. Everyone has a role to play in the delivery of Best Care, and the team at Grant Lodge do this incredibly well!
EMR 2.1 successfully done

It was a very busy month during July as Phase 2.1 of our EMR successfully went live across our Sunshine, Williamstown, Sunbury and Footscray Hospital sites!
The roll out has involved the Emergency Departments, Theatres, Newborn Services, Specialists Clinics, Cancer Services and Intensive Care Units transitioning to the EMR Phase 2.1 functionality to facilitate and document patient care. This project also involves continuing the rollout to Maternity and other important optimisation work over the next few months.
A huge thank you for the exceptional collaboration and enthusiasm we witnessed over the Go-Live period. Thank you to the thousands of staff who completed training and then practiced and prepared ahead of the Go-Live. The level of energy and commitment in the lead up to the Go-Live was extraordinary.
A super special thank you to the over 1,000 EMR Super Users who put their hands up to be upskilled to support their colleagues throughout the roll out and beyond! We’re so proud of this dedicated and talented group.
Finally, a very big thank you to the Digital Health Team who commenced the development of the EMR Phase 2.1 project four years ago. Many other teams from across Western Health also provided considerable support in the lead up to and throughout the Go-Live including Digital Technology Services, Biomed Engineering, Best Care Co-ordinators, Reporting and People Services.
The official EMR Go-Live support period recently finished and the rostering of Super Users who are focused on EMR support has concluded, with the exception of Specialists Clinics Medical Officer Super User support which will continue until Friday 11 August.
While the EMR Super Users are now undertaking their usual workloads, they remain the integral ‘Go-To’ support people as you continue to adapt to the new digital landscape. If you have a query, please seek out a Super User from your area and also please remember the availability of the Quick Reference Guides on the Digital Health information site.
To provide further support to the Super Users, the EMR Team’s dedicated support line will continue to operate from 7:00am to 5:00pm until this Friday 4 August at which point it will be reviewed. The EMR Team will also continue to monitor the EMR Go-Live Slack channel Monday to Friday from 8:00am to 5:00pm until mid-August.
Enterprise Agreement preparations underway

The Nurses and Midwives (Victorian Public Health Sector) (Single Interest Employers) Enterprise Agreement 2020-2024 will expire on 30 April 2024, and the Victorian Public Mental Health Services Enterprise Agreement 2020 -2024 will expire on 31 December 2024.
Processes are underway in readiness to negotiate the next nurses and midwives agreement and will be repeated again for the mental health agreement.
Logs of Claims:
We are up to this point at the moment. Both employers and unions are finalising their respective logs of claims. These documents are essentially the list of ‘asks’ for consideration as part of the negotiation.
Unions develop their log of claims through resolutions at delegates conferences and consultation with their members, as well as their knowledge and experiences over the past few years of the current agreement. Once finalised, unions publicise their log of claims to their members.
The employers, who are represented by the Victorian Hospital Industrial Association (VHIA) develop their log of claims through consultation with managers of health services through different meetings and forums. Again, the employers will call upon their knowledge and experience over the past few years of the current agreement. The Employer Log is informed by the State Government’s wage policy, and the Government (via the Department of Health) oversees and approves the strategy and negotiations for all major enterprise agreements.
Negotations:
Once the Logs of Claims are finalised, the parties come together to try to negotiate an outcome.
Invariably there will be some things in the Logs of Claims where the parties want a similar outcome, and others where there are differences. The parties work through each other’s ‘asks’ to negotiate, compromise and work through details of how elements may be enacted within the enterprise agreement and how to decrease the likelihood of unintended consequences.
The success of these negotiations and how close the parties are in their positions influences whether or not the unions enact their right to take industrial action.
As this process progresses over the coming months, we will keep you informed.
Become a health and wellbeing champion

The Nursing & Midwifery Health Program Victoria (NMHPV) recently announce that registrations are now open for the ‘2023 NMHPV Champion Training’ program!
The training is planned as an in-person event. Each date is a separate, one-day experience identical in nature, being held in Melbourne and Ballarat.
The ‘NMHPV Champion’ initiative, is a peer engagement and training model. It is designed to raise awareness of NMHPV and how to promote the health and wellbeing of our colleagues and professions.
A small fee of $49.50 will apply, this gives the participant the training package, a tailored individual self-care program which is transferrable to the workplace or the home, a delicious morning tea, lunch and attracts 5 CPD points.
All nurses, midwives, students, health service leaders and human resource personnel from Melbourne and the Ballarat region are invited to participate in this interactive training.
For more information please click here.
Melbourne
ANMF Victoria Branch – Carson Centre
Friday 20th October 2023, 9.30am to 3.30pm
Registration opens at 9.00am
535 Elizabeth Street, Melbourne Victoria 3000
Melbourne Tickets: https://www.trybooking.com/CJWGP
Ballarat
Mercure Hotel Ballarat
Friday 27th October 2023, 9.30am to 3.30pm
Registration opens at 9.00am
613 Main Rd, Ballarat VIC 3550
Ballarat Tickets: https://www.trybooking.com/CJWGN
Farewell Helen

Helen Sinnott, Director of Nursing & Midwifery, Sunshine recently announced that she is resigning from Western Health to take up a new position as the Clinical Health Executive at Oracle Health (Cerner).
Helen joined Western Health in February 2017 as the Chief Nursing and Midwifery Informatics Officer and was appointed as the Director of Nursing & Midwifery (Sunshine Hospital) in July 2021.
Helen’s leadership, passion and engaging approach has shaped nursing and midwifery informatics and professional practice at Western Health, and she has been integral to the implementation and adoption of both Phases 1 and 2.1 of the EMR across Western Health. Helen was also instrumental in our COVID-19 pandemic response, and she has been a strong and respected member of the nursing and midwifery executive team throughout her time at Western Health.
Well respected by colleague and stakeholders both within Western Health and beyond, Helen will be missed. A huge thank you to Helen for her commitment, leadership and her support throughout her time here at Western Health.
Helen will finish with us on 13 October 2023. I know you will join me in congratulating Helen on her new appointment and wish her every success.
Aboriginal nurse and midwife post-graduate scholarships close soon

Western Health and the Victorian Government is committed to supporting and strengthening the Aboriginal health workforce which will help to deliver improved health outcomes for Aboriginal people.
As part of this ongoing commitment, the Aboriginal Postgraduate Scholarship program for Aboriginal nurses and midwives will continue in 2023-24.
The expression of interest processes for Aboriginal nurse and midwife postgraduate scholarships for 2023-24 are now open.
For your information, please view the Expression of Interest and Guidelines for the Aboriginal Nursing and Midwifery Postgraduate Scholarship Program 2023-2024
Please send completed expression of interest forms to Debra.Broomfield@wh.org.au by 4 August 2023, to allow time for Western Health to review, endorse and submit to the Department of Health by the 11 August deadline.
Getting ready for Accreditation

Then any time between 1 July 2023 and 31 December 2023, a short-notice assessments will be undertaken for all of Western Health with 24 hours notice. Our mental health services will be included in our survey. We will be notified on a Thursday that a week long survey will commence on the next Monday.
We will have a team of approximately 11 accreditation surveyors visiting all of our campuses and over a week. The surveyors will spend up to 75% of survey time in clinical wards and departments.
Dame Phyllis Frost Centre will align with the new Primary & Community Health Accreditation Scheme that has a scheduled, separate accreditation survey.
What can I do to be ready?
To get ready, as you are working in your department try to look through a surveyor’s eyes:
- remove outdates or unnecessary posters and information on walls
- get rid of excessive clutter
- ensure WOW drawers are locked and are clean inside
- ensure linen trolleys are always covered
- ensure that equipment that has been cleaned has a green tag on it
- ensure cleaning schedules are visible
- ensure daily checks eg resuscitation trolley are recorded
- ensure you are able to confidently navigate the EMR in front of a surveyor
- make sure that medication and sterile stock rooms are always cleaned
- maintain a focus on the privacy of patient information
Over the coming months we will be focusing on ensuring consistency of practice across out departments, to ensure that we are all delivering Best Care everywhere, every time.
Riskman upgrade

In response to recommendations from the report, “Targeting zero, the review of hospital safety and quality assurance in Victoria” the Department of Health has implemented changes to the incident reporting requirements for public health services in Victoria.
An early warning reporting system aimed at identifying emerging risks for both patients and the healthcare workforce is being implemented throughout the state. The system will contribute to enhancing safety and quality measures in healthcare delivery that relies on near real-time data submission.
To support the real-time data submission changes, the Western Health Riskman system will undergo an upgrade on Tuesday 1 August 2023. It is anticipated that the system will be unavailable for approximately 2 hours on this day.
Key changes for the reporting and upgrade are:
- ISR 1 and 2 notification alerts: All ISR 1 and 2 alerts will be sent to users immediately upon incident submission. Any changes to ISR will be communicated to the Divisional Director by the aligned divisional Best Care Coordinator. Please refer to the Determining ISR QRG for details on accurately assigning the ISR for clinical incidents.
- Incident review timelines: Incidents will be considered valid for inclusion in reporting to the Department of Health 30 days from incident submission into Riskman. We will need to conduct timely reviews during incident investigations to ensure data accuracy and completeness with 30 days.
- Riskman appearance: There will be a change in the overall appearance of Riskman.
- Sexual behaviour incidents: Sexual behaviour incidents will no longer default to ISR 2 upon incident submission.
- Default selection removed for ‘Event relates to’ field: Users will have to select the ‘Event type’ when entering an incident.
- Warning Messages when closing an incident: To ensure data sent to the Department of Health is complete and accurate, users closing an incident will see a new warning message prompting them to check all mandatory fields prior to submission.
Further detail on the changes is available on the Live Best Care Microsite. The Best Care Governance and Support division will be available to support staff following the upgrade. If you have any queries, please contact the Riskman Help Desk via email or your Best Care Coordinator.
Baxter 0.9% Sodium Chloride bag shortage

There continues to be nationwide shortages of Baxter 0.9% Sodium Chloride 100 mL and 1000 mL IV bags.
Western Health will be using 100 mL and 1000 mL Baxter IV bags imported from the USA, as permitted under Section 19A of the Therapeutic Goods Act.
The S19A USA products are identical in active ingredient and strength to the TGA registered Australian products. Key differences are highlighted below.
Of significance is the pull off port protector (blue colour) on the S19A USA Baxter bags.
All staff must ensure that proper aseptic technique is followed when spiking the port.
Once the blue pull-off port protector has been removed, you can attach the giving set using a twisting motion to spike the port.
S19A Baxter USA 100 mL and 10000 mL IV bags will be supplied to all clinical areas in the coming days.
Once the shortage is resolved, all areas will return to TGA registered Baxter bags as usual.
Let's Talk Leadership

The Australian College of Nursing Institute of Leadership is proud to announce the Let’s Talk Leadership series. The series highlights high profile leaders, who share their triumphs and lessons learnt. The nest session is in Melbourne on Tuesday 29 August 2023 from 5:30pm to 8:30pm.
The keynote speaker for this event is Professor Greg Hunt, who was appointed Honorary Enterprise Professor in the Faculty of Medicine, Dentistry and Health Services and the Faculty of Business and Economics at the University of Melbourne in December 2022. Greg is also the inaugural Chair of the Advisory Council for the Turner Institute for Brain and Mental Health at Monash University. He advises a wide range of businesses and not for profits in the areas of innovation, leadership, strategic planning, health and the environment.
Greg is a highly experienced former Cabinet Minister in the Australian Government, having served as Australia’s Minister for the Environment, Innovation and Health across three major portfolios over almost nine years.
Registrations to this event are exclusive to ACN Members and registration is free. Members may bring a non-member as a guest, limited to one guest per member. To register please click here.
ACN's National Nursing Forum

The Australian College of Nursing’s signature annual nursing event, the National Nursing Forum (NNF), will take place in Adelaide from Wednesday 9 – Friday 11 August 2023.
The event will inspire and reinvigorate you through presentations, panel discussions, networking with high-profile leaders, and opportunities to connect and socialise with like-minded nurses. It includes:
- Speed Leaders Session: Think speed dating but for professional conversations! The Speed Leaders Session enables delegates to have short, sharp conversations with experienced nurse leaders to gain knowledge and advice first-hand. Our Speed Leaders are renowned experts in their fields.
- Gala Dinner: The Gala Dinner allows delegates to take a break from stimulating their grey matter and let their hair down! A highlight of the event, the Gala Dinner is the perfect opportunity to get dressed up, enjoy tasty treats and exciting entertainment, and dance the night away with colleagues from around the country.
- Oration, Investiture & Award Ceremony: This prestigious component of the NNF incorporates an Oration speech presented by an esteemed leader, the Investiture of new ACN Fellows who are being recognised for their contributions to the profession and ACN, and the presentation of ACN Grants and Awards which support nurses to pursue study and research.
- Poster Presentation: The Poster Presentation provides a unique opportunity to learn about ground-breaking nursing research, ask questions directly to the authors and have your say by voting for the best poster.
- Panel discussions: Panel discussions are an engaging way for a group of experts to exchange insights and opinions. This year’s NNF will feature panel discussions with Health Minister’s Award for Nursing Trailblazers Finalists and ACN Board members.
- Networking events: The NNF attracts some of the brightest nursing minds from all corners of Australia and the event offers numerous networking opportunities allowing you to make invaluable connections, build your profile and seek advice.
- Workforce Strategy Breakfast: The Workforce Strategy Breakfast provides a platform for nurses from various settings, career stages and geographic locations to get together to discuss challenges facing the profession and collaboratively brainstorm solutions.
- Faculty sessions: ACN offers 24 Faculty groups, including Aged Care Nursing, First Nations, Leadership and Military Nursing, allowing members to connect with peers who share similar areas of interest or practice. The Faculty sessions during the NNF are a unique opportunity to meet face-to-face with members of Faculties you belong to and find out more about Faculties you are interested in joining.
Tickets to the must-attend event are still available. If you won’t be able to go to Adelaide, don’t worry, you can register to attend the virtual event.
Seeking frontline healthcare workers for the SCV Health Innovators Program

Safer Care Victoria is aware of the very significant challenges currently facing healthcare providers across the Victorian healthcare system. In the face of these challenges there is a critical push and a growing interest in healthcare innovation across the sector. With exponential advances in healthcare innovation and the high level of expertise in our healthcare workforce there is great potential for frontline healthcare workers to co-create solutions to persistent healthcare problems impacting on patient safety and health equity.
Healthcare innovation is about applying new or novel solutions to healthcare problems. It involves piloting and testing new solutions at a local level on a small scale before they are recommended for embedding scaling and spreading through a healthcare improvement model. It is distinctly different to healthcare improvement which is about improving existing systems, processes, and tools to solve problems in healthcare (using known best practice).
In collaboration with the Institute of Health Improvement, Safer Care Victoria has developed a Health Innovators to build innovation capability and support innovation across the healthcare sector. The program consists of 5 learning modules, along with fortnightly coaching and mentoring sessions from international experts in the health innovation sector. Participants will be supported to implement an innovation project throughout the program. The project will focus on exploring a healthcare problem that is impacting on patient safety and health equity, and in finding innovative solutions to that problem. The program will run from September 2023 to February 2024.
Interested candidates are required to complete a short 3 minute ‘shark tank’ style video explaining what their healthcare problem is and why it needs an innovative solution. Candidates with successful videos, will be invited to submit a further short written brief to support your idea and inclusion in the Program. Further details of the program and the application process are available in the program’s flyer.
Candidates may submit their video EOI to innovation@safercare.vic.gov.au by 14 August 2023 to be considered for this program.
Still not Flu Vax'd?

A reminder that the annual Flu Vax is now legally mandatory for all Category A and B healthcare workers. Category A and B healthcare workers are those that:
- have direct physical contact with patients, clients, deceased persons or body parts, blood, body substances, infectious material or surfaces or equipment that might contain these; or
- have contact that might allow respiratory infections to be acquired or transmitted, which includes workers with prolonged face-to-face contact with patients or clients or where their normal work is in a clinical area.
All these staff are required to receive the flu vaccine prior to 15 August 2023 to ensure that they meet their legal obligations and the requirements of their employment contract with Western Health.
As Western Health’s flu vaccination program has now finished, any unvaccinated Category A or B staff need to undertake one of the following 4 actions:
- Yet to receive the flu vaccine in 2023: these staff are now responsible for getting the vaccine via their General Practitioner or local Pharmacy at their own expense. Once you have received the vaccine you must complete our Influenza Immunisation Survey and attach your vaccination certificate available through your Medicare webpage prior to 15 August 2023.
- Already received the flu vaccine elsewhere in 2023: It is important that our records are updated to reflect every staff member’s vaccination status. To do this, you must complete our Influenza Immunisation Survey and attach your vaccination certificate available through your Medicare webpage prior to 15 August 2023.
- Have valid medical reason to seek a medical exemption: The only reasons you may be able to get a medical exemption from having the flu vaccine are if you:
-
- Had anaphylaxis after a previous dose of any influenza vaccine
- Had anaphylaxis due to any vaccine component within the influenza vaccine
- Have a history of Guillain-Barré syndrome within 6 weeks following a previous dose of influenza vaccine (unless an alternative cause has been clearly identified).
If you are seeking an exemption for the influenza vaccine, you must complete our Influenza Immunisation Survey prior to 15 August 2023.
- Should not be classified as a Category A or B healthcare worker: If your role does not meet the above definition, please contact our Infection Prevention team via email Flushot@wh.org.au and outline the reasons why you believe this to be the case, and please copy in your manager.If you are a Category C staff who is refusing the vaccination, you still must complete your declaration via our Redcap survey Influenza Immunisation Survey. Western Health is required to report back to the Department of Health the number of Category C staff that have refused the vaccine.
Please be advised that if you have not met the requirements as outlined above by 15 August 2023, Western Health is legally obliged to undertake a Risk Assessment to review your role and the risks posed within the workplace whilst you are unvaccinated, and whether you will be able to meet the inherent requirements of your role at Western Health.
Benchmarking Best Care
The latest benchmark reports from the Health Roundtable that go up to March 2023 show how our delivery of Best Care compares to other health services across Australasia.
Let’s look at how we perform in the area of hospital acquired infections. Hospital acquired infections include urinary tract infections, surgical site infection, pneumonia, blood stream infection, central line and peripheral line associated bloodstream infection, multi-resistant organisms, infection associated with prosthetics/implantable devices, gastrointestinal infections and other high impact infections.
Hospital Acquired Infections:
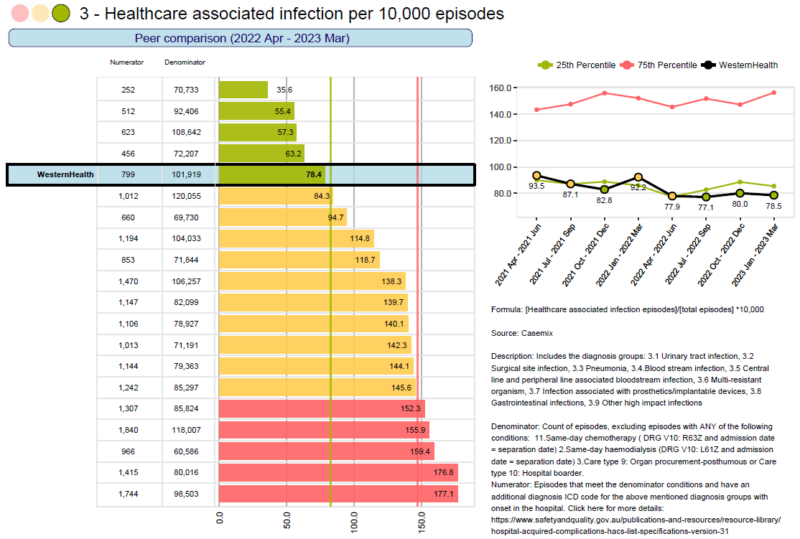
The rates of hospital acquired infections at Western Health is in the green and has been trending downwards.
Well done everyone!
This means that our patients get far less hospital acquired infections that we do at peer hospitals. This is a wonderful result.
Remember, you can impact these results through:
- Gloves should always be clean: gloves should always be changed between patients, and clean gloves are always required when undertaking any procedure. Hand hygiene is required between changes of gloves, and alcoholic hand rub must never be applied to gloves.
- Hand Hygiene: ensure you undertake the 5 moments of hand hygiene and that there is alcoholic hand rub present at every bed side and point of care.
- Correct skin preparation: whenever an invasive device is being inserted, chlorhexidine skin preparation must be utilised. An alcohol wipe is never an appropriate skin preparation.
- Antiseptic non-touch technique (ANTT): when inserting, accessing, dressing or removing any invasive device, ANTT needs to be utilised. Also please ensure that you use a clean stainless steel dressing trolley, not a kidney dish, bedside table or the patient’s bed.
- Only insert a device if it is needed: Always ‘hesitate before you cannulate’. Does the patient really need that device inserted? Never insert a device ‘just in case’. Any invasive device is a potential source of infection, so let’s minimise them where we can.
- Remove the device as soon as it is not needed: As soon as a device is no longer needed, remove it as quickly as possible. Ask medical staff to change IV orders to oral orders where appropriate. The longer devices are in situ, the greater the risk of an infection occurring.
Educational Opportunities

Resuscitation Mandatory Competencies:
Sessions have recommenced. In the first instance, you can arrange an assessment with your local instructor or educator. Resus educators are contacting managers to arrange local sessions for individual teams. Dedicated sessions for Bank and Pool Staff along with sessions for Nursing and Medical staff are available on WeLearn. You can locate sessions by clicking on this link: Course: Basic Life Support (BLS) (wh.org.au)
Invasive Lines & Cannulation:
Dates for Bank-Pool Nursing staff, Ward Nursing staff, Radiology, and Medical staff available soon.
Adult Deteriorating Patient (non-obstetric):
Learning how to recognise and escalate patient deterioration is now here at Western Health. The Education and Learning Department have developed a new and improved WeLearn course, designed to guide and support early recognition and escalation for a patient deteriorating within Western Health.
Fisher and Paykel Respiratory Support training:
RSVP to: education.australia@fphcare.com.au
- Infant Respiratory Support: Friday 1 September 2023 – WCHRE Auditorium: 9.00am to 3.00pm
- Adult & Paediatric Respiratory Support: Wednesday 4 October 2023 – WCHRE Lecture Theatre: 9.00am to 1.00pm
Education and Learning upcoming events:
- 05/09/2023: Cognitive Study Day
- 21/09/2023: Infection Prevention Study Day
- 27/10/2023: Mental Health First Aid
- 03/11/2023: Mental Health First Aid
More courses click here: Courses and Inservices (westernhealth.org.au)
Course Enrolment/Inquiries:
- WeLearn Helpdesk Email: welearn@wh.org.au
- WeLearn Enrolment link: welearn@wh.org.au
Emerging Evidence
The Western Health Library Service is a great source for locating the latest nursing and midwifery related evidence-based practice and research.
Latest articles of interest:
- Preconception factors associated with postnatal mental health and suicidality among first-time fathers: results from an Australian Longitudinal Study of Men’s Health. Social Psychiatry and Psychiatric Epidemiology. 2023: August. Full Text Western Health Author
- The green maternity project: a midwife-led initiative to promote correct waste segregation on an Australian postnatal ward. Journal of Advanced Nursing. 2023: July Full Text Western Health Author
- Nurses’ work experiences in hospital wards with single rooms: an integrative review. Journal of Clinical Nursing. 2023: July Full Text Western Health Author
- Letter to editor. Journal of Advanced Nursing. 2023: July Full Text Western Health Author
Australian Library & Information Week 31 July – 6 August 2023
This week we celebrate Western Health Library’s information services and offer a range of useful information seeking tools. To help you get started on EndNote and Covidence, we have added two NEW group sessions for Library and Information Week.
New Nursing/Midwifery eBooks
- Clinical practice guidelines for midwifery & women’s health. 6th ed. Jones & Bartlett Learning, 2022
Clinical Practice Guidelines for Midwifery & Women’s Health, Sixth Edition remains an accessible and easy-to-use quick reference guide for midwives and women’s healthcare providers. Thoroughly updated and revised to reflect the changing clinical environment, it offers current evidence-based recommendations, updated approaches, and opportunities for midwifery leadership in every practice setting. The Sixth Edition features new information on diversity and inclusion, sexual health, opioid disorder and substance-exposed newborns, care for the individual who is transitioning and after transition, and more timely and relevant topics.
View all recently added print and eBook catalogue titles
Accessing the Library at Work:
All eligible staff can access electronic library resources from any networked PC or device connected to
Wi-Fi network without the need to login.
Accessing the Library Remotely (offsite access):
- When accessing electronic resources through the library website from offsite you will automatically be asked to enter your library membership number and surname.
- Library Membership is free and can be completed online. Please email the library if you experience issues when registering (e.g. error messages).
For more information please contact the Western Health library team.

