Published on 1 November 2023
Edition 73: November 2023
-
Helpful contacts
Employee Assistance Program: 1800 099 444
Nurse & Midwife Support: 1800 667 877
Nurse & Midwife Health Program: 03 9415 7551 or 1800 888 236
-
Upcoming dates
November 2023
5 ACN’s Emerging Research Leader program applications close
7 Melbourne Cup Day
8 Best Care Week commences
8 Auditing Best Care Day
10 Best Care Awards webinar
11 Remembrance Day
13 Reflection and Recovery Week commences
15 Inspire Awards live stream
16 RedCAP Advanced Workshop20 Launch of OVA Predict, Prevent, Prioritise: Safety at Bacchus Marsh Hospital
22 Nursing & Midwifery Grand Round (2pm)
30 Co-design Methodology WorkshopCheck out Events for more details.
-
Nursing & Midwifery Executive
Adjunct Professor Shane Crowe
Executive Director of Nursing & Midwifery
Phone: 8345 1463
Email: shane.crowe@wh.org.auProfessor Bodil Rasmussen
Chair of Nursing, Deakin University/Western Health
Phone: 8395 8163
Email: bodil.rasmussen@wh.org.auDoug Mill
Director of Nursing & Midwifery
Division: Chronic & Complex Care
Phone: 0400 807 938
Email: douglas.mill@wh.orh.auAdjunct Associate Professor Jo Mapes
Deputy Executive Director of Nursing & Midwifery
Phone: 0423 302 337
Email: joanne.mapes@wh.org.auKylee Ross
Acting Director of Nursing & Midwifery Informatics (CNMIO)
Phone: 0409 555 384
Email: kylee.ross@wh.org.auLena Pejcinovski
Director of Nursing, DPFC
Division: Custodial Health
Phone: 0422 818 187
Email: lena.pejcinovski@wh.org.auProfessor Linda Sweet
Chair of Midwifery, Deakin University/Western Health
Phone: 8395 1178
Email: linda.sweet@wh.org.auLisa Gatzonis
Director of Nursing & Midwifery Workforce
Phone: 0466 943 769
Email: lisa.gatzonis@wh.org.auMichelle Read
Director of Nursing & Midwifery
Division: Perioperative & Critical Care
Phone: 0466 618 966
Email: michelle.read@wh.org.auMonique Sammut
Director of Nursing & Midwifery, Sunbury
Divisions: WPHU and Clinical Support & Specialist Clinics
Phone: 0412 769 423
Email: monique.sammut@wh.org.auNicole Davies
Director of Nursing & Midwifery, Williamstown
Division: Emergency, Medicine & Access
Phone: 0435 656 190
Email: nicole.davies@wh.org.auRobyn Peel
Director of Education & Learning
Phone: 0468 608 141
Email: robyn.peel@wh.org.auRohan Vaughan
Director of Nursing & Midwifery, Melton
Division: Drug Health
Phone: 0434 365 769
Email: rohan.vaughan@wh.org.auRyan Dube
Director of Nursing
Division: Mental Health & Wellbeing
Phone: 0420 228 035
Email: ryan.dube@wh.org.auAdjunct Professor Tanya Farrell
Deputy Executive Director of Nursing & Midwifery/Director of Maternity Services
Division: Women’s & Children’s
Phone: 0468 830 755
Email: tanya.farrell@wh.org.auVal Dibella
Director of Nursing & Midwifery
Division: Best Care Governance & Support
Phone: 0466 489 687
Email: val.dibella@wh.org.auWendy Giddings
Director of Nursing & Midwifery, Bacchus Marsh
Division: Aged, Cancer & Continuing Care
Phone: 0458 603 897
Email: wendy.giddings@wh.org.auWendy Watson
Deputy Executive Director of Nursing & Midwifery
Phone: 0478 305 046
Email: wendy.watson@wh.org.au
From Shane

We have had an incredible past few years, and there has not been a shortage of major areas of focus that have impacted upon our nurses and midwives. To name a few – we became designated mental health service, took over the provision of primary healthcare with women’s custodial services, implemented the second phase of our EMR, welcomed our Bacchus Marsh and Melton colleagues into Western Health, expanded Sunshine ED, have been planning and building a number of major new hospital developments and unfortunately, we were the most impacted health service in the country from COVID. Over these years we have also grown by approximately 60% to meet the needs of our community, welcoming many new nurses and midwives to the Western Health team.
I am enormously proud that despite these significant events and competing priorities, our nurses and midwives have continued to maintain a focus on the quality and safety of the care that we provide. You have actively participated in local and organisational improvement initiatives, which has resulted in a continual reduction in the rate of hospital acquired complications and serious adverse events.
Our short-notice accreditation survey is now imminent, and highly likely to occur sometime this month. An enormous amount of work has been put into preparing for this accreditation, and I would like to thank you all for the significant effort and support that you have shown in optimising the way we work and refining our practices and systems to enhance Best Care to our consumers.
You should feel rightfully proud of this work. If you have the chance to talk to the surveyors as they travel around our health service, it is a chance for you to describe with pride the important work that you do every day in delivering Best Care. They are not here to trick you – they will genuinely want to hear about what you do and how your team has continued to improve. Think back over the past few years, and there will be lots of examples of how this has occurred.
To deliver Best Care, you need the best nurses and midwives. I sincerely believe that this is the case at Western Health. We have got this, and you will be brilliant! I am very grateful to you all.
Our annual Quality Account publication outlines how Western Health – in partnership with our consumers, their families and carers continues to strive for our vision of Best Care. After a hiatus during COVID-19, we are back to producing this publication annually. The Quality Account 2023 showcases a range of improvements and projects undertaken to enhance Best Care over the past year, in an environment where providing person-centred, coordinated, safe and right care for a rapidly growing population with complex health needs has been incredibly challenging. This is a testament to the commitment of all staff to provide Best Care every time, with every consumer, everywhere!
It was wonderful to see the quality, depth and scope of nurse-led and midwife-led research during Research Week last month. Congratulations to all of our presenters and to the recipients of the Nursing & Midwifery Research Grants for next year. It was also an opportunity to acknowledge and celebrate the amazing legacy that will be left by our outgoing inaugural Chair of Nursing Professor Bodil Rasmussen during her last Research Week with us, prior to her finishing up with us at the end of the year.
Over the next few weeks we will release the nominations for the annual Nursing & Midwifery Excellence Awards, which will be celebrated during December to finish off 2023 on a high. Now is a great time to start to consider the individuals and teams that you think should be recognised and rewarded, so you can put in your nominations when they are released.
Finally, a number of excellent events are being held this month, including our Inspire Awards, Best Care Week and Reflection and Recovery Week. I hope you can find some time in your busy days to participate in these positive and affirming events.
Shane Crowe
Executive Director, Nursing & Midwifery
Accreditation: we are ready!

It is likely short-notice accreditation survey will happen during November 2023. We will be notified on a Thursday that our accreditation survey will be start on the following Monday, and it will run all week.
How will staff be notified when there will be an accreditation survey and what do we do next?
We have developed a plan to activate when we are given our 24 hour notice that Accreditation Surveyors will be visiting Western Health. Note: We will be given notice on a Thursday, with a Survey commencing on the Monday and concluding on the Friday.
This plan includes a number of ways to notify staff, services and patients, including emails, PA announcements and screen savers.
All staff communication will tell staff to access the home page of the Live Best Care site. A big banner with a link to Accreditation Survey roles for staff, FAQs and tools will be visible to support you through the Accreditation Survey.
The link will take you to the following page which will be updated when survey is announced: NSQHS Accreditation Survey FAQs and Tools – Live Best Care (wh.org.au)
Final preparation:
Over the past few months we have focused on areas identified during our June mock accreditation survey where our practices or processes could have been improved. This includes decluttering of clinical areas, consistent use of 3 points of patient identification and utilising the EMR to support consistent clinical handover practices. The work done has been fantastic, and well done to everyone on making these improvements.
The Live Best Care Microsite is our central information portal for staff on our Quality Systems supporting Best Care and compliance with National Standards. The section under ‘Accreditation’ – ‘Are you ready for NSQHS Accreditation?’ … contains FAQs and links to resources to help staff feel ‘Accreditation Ready’.
Due to everyone’s collective efforts, we are now ready for accreditation – and a huge thank you to everyone. You can talk to the surveyors with confidence that we deliver Best Care to every person, everywhere and every time.
Lots of effort has been put into changing our systems so that from now we will remain accreditation-ready, so that we will be confident when any short-notice assessment occurs in the future.
Congratulations to our new DONMs
In what was a highly competitive field of internal and external applicants, I am delighted to announce the appointment of Michelle Read and Val Dibella as Directors of Nursing and Midwifery.

Michelle has worked at Western Health within the Nursing & Midwifery Workforce Unit for the past 4 years as the Deputy Director where she has overseen the operations of the unit as well as implementing workforce goals and objectives. Michelle has extensive experiencing in managing nursing and midwifery professional and industrial matters, and implementing organisation-wide initiatives. Michelle’s previous roles include her being instrumental in the implementation and adoption of Phase 1 of the Electronic Medical Record. Michelle is committed to the provision of best care for our consumers and the professional development of our nurses and midwives. Michelle will be the Director Nursing & Midwifery for Footscray Hospital and will work in partnership with the Perioperative & Critical Care Division. She will commence in her new role on 11 December 2023.

Val has had a long association with Western Health, predominately working within the Centre for Education where she led our maternity, paediatric and neonatal education programs, our WeLearn team and also acted as the Director of Education & Learning. For the past 7 months, Val has been acting as a Director of Nursing & Midwifery where she has implemented multiple improvement projects and has enhanced our leadership programs for our Associated Unit Managers, Unit Managers, Nurse Practitioners and Clinical Nurse Consultants. Val will be the Director Nursing & Midwifery for Sunshine Hospital and for the moment will focus on supporting Comprehensive Care. She will commence in her new role on 30 October 2023.
I am delighted that 2 internal candidates have been successful in these highly sought-after roles. Please join me in congratulating Michelle and Val and wishing them every success.
Celebrating Nurse and Midwife-led Research
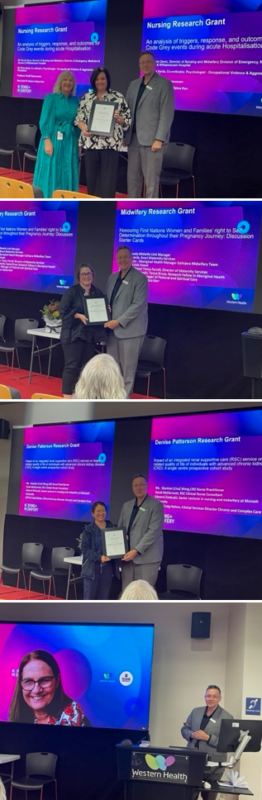
On Tuesday 19 October 2023 as part of Western Health’s Research Week, the Nursing & Midwifery session was held in front of a good in-person and on-line audience to celebrate nurse-led and midwife-led research.
Our key note speakers for the session were Associate Professor Debra Kerr and Adjunct Professor Tanya Farrell.
Debra is relatively new to the Western Health-Deakin University Partnership, and gave a really interesting overview of her past research and findings – including her specialisation in nursing communication and intranasal Naloxone.
Tanya gave an inspiring address on the importance of midwives within the health system, changes to the midwifery workforce over time and how midwives can influence the future from ward, boardroom and beyond!
At the session Adjunct Professor Shane Crowe awarded the Nursing & Midwifery Research Grants for 2023. The recipients were:
Nursing Research Grant ($15,000): Was awarded to ‘An analysis of triggers, response, and outcomes for Code Grey events during acute Hospitalisation‘. The research team is Nicole Davies (DONM), Elisa Ilarda (Operations Manager, OVA Program), Associate Professor Debra Kerr, Dr Adam Searby and Professor Bodil Rasmussen.
Midwifery Research Grant ($15,000): Was awarded to ‘Honouring First Nations Women and Families’ right to Self-Determination throughout their Pregnancy Journey: Discussion Starter Cards‘. The research team is Cara Kennedy (Midwife Unit Manager), Karah Edwards, (Koori Maternity Services Worker), Jordan Casey (Aboriginal Health Manager), Galinjera Midwifery Team, Professor Linda Sweet, Adjunct Professor Tanya Farrell, Dr Vidanka Vasilevski, Tanya Druce (Research Fellow in Aboriginal Health), Sacha McDonald (Manager of Pastoral and Spiritual Care) and Associate Professor Debra Kerr.
Denise Paterson Research Grant ($10,000): Was awarded to ‘Impact of an integrated renal supportive care (RSC) service on health-related quality of life of individuals with advanced chronic kidney disease (CKD): A single centre prospective cohort study‘. The research team is Lisa Wang (CKD Nurse Practitioner), Sarah McDermott (RSC Clinical Nurse Consultant), Edward Zimbudzi (Senior Lecturer at Monash University) and A/Prof Craig Nelson (Clinical Services Director Chronic and Complex Care).
At the session we also took the opportunity to acknowledge the amazing legacy that will be left by our outgoing inaugural Chair of Nursing Professor Bodil Rasmussen (pictured right). Bodil has been Western Health’s inaugural Chair of Nursing, and over the past 7 years Bodil has made a remarkable and long-term positive impact on nursing at Western Health. Her leadership, passion and approach has supported our nurses to significantly grow their research capability and critical thinking.
Bodil’s achievements over her time at Western Health are truly amazing, with our nurses now publishing on a monthly basis, regularly presenting at conferences, compiling posters and undertaking projects in a robust way. Bodil has connected our nurses with academic colleagues from across the world, making for excellent opportunities to learn and collaborate. None of this would have been possible without Bodil!
Bodil will finish in her role on 31 December, and she has agreed to support the transition of her successor. The process to appoint our next Chair in Nursing is currently underway.
Focus on the use of bed rails
![]()
Did you know that bed rails are considered a Type 2 restraint when they are used to intentionally prevent a person from getting in and out of bed? This is still the case if a person (or their medical treatment decision maker) requests or consents to their use, and when used in an emergency.
Historically, bed rails were used in hospitals as a form of patient safety, however we now understand that patients are often at greater risk of serious injury if bed rails are used. Western Health endorses the Safer Care Victoria guidelines on use of bed rails in hospital and this is reflected in Western Health’s Preventing Patient Falls and Harm from Falls PPG.
To summarise, at Western Health, bed rails can be used only if the patient remains closely monitored and are:
- Being transported on a bed or trolley.
- Recovering from anaesthetic and is not yet fully alert.
- Temporarily to help with bed mobility – for example, to help the person to reposition.
- A bed rail can remain in place on one side of the bed to assist with bed mobility if requested by a cognitively intact patient.
- A current inpatient in the Intensive Care Unit being nursed in an ICU/HDU model of care.
At Western Health, bed rails must not be used:
- Against a patient’s wishes.
- As a form of restraint.
- When a person has delirium, is disorientated, agitated, impulsive or cognitively impaired.
- When a person can mobilise safely and independently, unless the person has requested to use bed rails.
What to do when a patient and/or family requests to use bed rails:
- If the patient has cognitive capacity and requests bed rails, you are obliged to use them even if it goes against your advice.
- A person and/ or their Medical Treatment Decision Maker (MTDM) may request bed rails to prevent the patient from falling from the bed, reduce fear of falling out of bed, or help with bed mobility or positioning. A MTDM cannot insist on the use of bed rails for a person who does not have capacity. This is because bed rails are not considered a medical treatment by law. The only exception is when the person is subject to an enduring power of attorney for personal matters that specifically authorises the use of bed rails.
In both of these situations, we recommend the request is escalated to the HMO and nurse-in-charge so they can:
- Talk the patient/family through risk of using bed rails (e.g. risk of entrapment, impalement or suffocation, reduced access to food/drink/toileting, injury risk trying to climb over rails) and explore alternatives to bed rails.
- Thoroughly document the person’s request, including the person’s acceptance of the risk.
- Make an appropriate plan to review the decision to use bed rails, if activated.
- Make a plan to reduce the risk when using bed rails, if activated.
There are many other interventions that can support your patient to be safe in hospital, please refer to Preventing Patient Falls and Harm from Falls procedure for more details.
New Sepsis Alert process in SHED
Sunshine Hospital Emergency Department is commencing a “Sepsis Alert” process for all patients who meet sepsis criteria – a multidisciplinary approach to timely antibiotics in sepsis – adults and paediatrics. The process will commence on 8 November 2023.
What does this mean – Identify, Communicate, Escalate, Activate
- After identifying sepsis, it is important that the bedside clinician (doctor or nurse), orders the “ED Adult/Paeds Sepsis” orderset on EMR so that 2 blood cultures and a lactate are requested.
- The patient must be communicated and escalated to the Nurse in Charge of your zone – if patient is in Wait Room/TAR or AV corridor – escalate to ED ANUM in main fish bowl.
- The NIC of the zone will escalate to ED ANUM who will activate the “Sepsis Alert” – a notification to relevant consultants, senior nursing staff and pharmacy staff.
The ED bedside clinician, should attend a bedside huddle – treating clinician, treating nurse and pharmacy (if on shift) – to check Best Possible Medication History, Allergies, and potential source of infection, and prescribe appropriate antibiotics (If TAR/AV Wait – NIC will arrange for appropriate cubicle space as soon as feasible). Pharmacy will assist the bedside nurse in preparation of and checking of antibiotics.
An audit undertaken between January to June 2023 showed only 36% of adult patients who met sepsis criteria received antibiotics within 1 hour, and our median time to giving antibiotics from prescribing was 39 minutes. With your help, we can reduce this time, and aim to improve compliance and hopefully patient outcomes, with a shared, multidisciplinary model.
Remember: IDENTIFY, COMMUNICATE, ESCALATE, ACTIVATE
SHED nurses can contact “Sepsis Alert” champions – Yasmin Sidiki (ED Senior Reg currently in Paeds) or Nicholas Kruse (ED Junior Reg) or Maurice Recinos (ED ANUM) for further information.
How have we improved? Let's ABC to see...

To support Western Health’s vision of best care, the Auditing Best Care (ABC) audit is a tool used to monitor our delivery of Best Care and provides us with an opportunity to identify areas for improvement on how we deliver that care.
ABC Day will be held across most inpatient areas across Western Health on Thursday 8 November 2023
The audit is to be completed at the following locations:
- All inpatient areas at Footscray, Sunshine, Williamstown and Bacchus Marsh Hospitals
- Emergency Observation Units (EOUs) at Footscray and Sunshine Hospitals
ABC Audit Day is held across most inpatient areas across Western Health every 6 months.
The audit tool is accessible via this link: Auditing Best Care: ABC Audit. There is also a video available on the Live Best Care microsite.
Each area is required to complete ¼ (one-quarter) of the total number of patients admitted to the ward on ABC Day. For example, a ward that has 30 patients admitted will be required to audit at least 8 patients.
To assist with random selection of patients to audit, click here to use a random number generator.
Our Language Services team are available to assist throughout ABC Day. Language Services can be contacted on ext. 57147 or 57148
The Best Care Governance and Support team will be available to assist on ABC audit day. Please reach out to your division’s Best Care Coordinator if you required assistance.
Reflection and Recovery Week
There is no doubt the last few years have been some of the busiest and disruptive of our people’s lives. We know this has taken a toll on many, and morale has suffered. In acknowledgment of the work that has been done and some of the sentiments of our people this year we will be holding Reflection and Recovery Week in the time normally assigned to Positive Workplace Week.
Our aim is that to better respond to needs, by asking some simple questions: – what’s causing pain at Western Health and collecting feedback.
We want to listen and seek feedback from our employees as well as suggestions of how to do things better, to enable Western Health to improve, achieve our goals and identify areas for improvement.
This is also a week to give those around you some positive feedback. Let people know you appreciate something they’ve done, whether it’s something specifically work related or for being kind, helpful or supportive. We want to acknowledge of our employees, who have continued to turn up every day during this period of significant change and new workflows, plus the additional demands associated with our many major projects.

People Matter Survey:
In the past, the feedback from staff has resulted in direct action to address workplace and cultural issues identified. This includes strategies and initiatives to improve engagement, connection, psychosocial safety and wellbeing, and skills based and leadership management capability development.
As a result of feedback from the 2022 survey, new policies to address fatigue management and flexible work options are currently in development.
We know that it is challenging to find time to participate, but it does provide an opportunity to have your say.
Here are some key details on the People Matter Survey 2023:
- The survey takes about 20 minutes to complete, and staff can complete it from October 30 until November 17.
- Launch week will feature pop-up stalls and give-aways at major sites.
- We use the de-identified feedback from the People Matter Survey to address any potential issues identified and to understand areas where we are hitting the mark. Each year our CEO Russell Harrison reads all the free text comments – last year there were around 3,000.
- There is a scorecard on the Westerly to help teams track their response rate against their peers and to help determine the divisional prize winners. There will also be individual prize raffles.
- The survey has strict rules to protect employee privacy and anonymity. Find out more here.
Advanced Care Planning

Advance Care Planning refers to the process that enables patients to plan for future medical care in case they will be too unwell to communicate their wishes in future. Advance Care Planning is one way we can support patients to receive medical care that is consistent with their values, goals, and preferences.
It involves:
- Appointing a Medical Treatment Decision Maker (MTDM)
- Discussing their goals and values around care with their MTDM
- Documenting the discussion on an Advance Care Directive
- Sharing this document with their treating team whenever they seek health care
On admission, all adult patients should be asked by their admitting nurse if they have an Advance Care Directive or Advance Care Plan and/or a Medical Treatment Decision Maker. This must be documented in the ‘End of Life Care’ Section of the ‘Initial Patient Assessment’ Power form.
If a patient has an Advance Care Directive or Plan and/or MTDM, they are required to provide Western Health with a copy of each. The Ward Clerk can add this information as an iPM alert and scan the documents into BOSSNET under the Alerts tab. The admitting nurse is required to add an alert into EMR. These documents may also be visible in My Health Record, accessible via the EMR.
Not all people are interested in Advance Care Planning. If a patient is interested, we must help them access the information they need. The Advance Care Planning process does require time and training, so we would not expect general staff to complete these with patients. However, you can point them in the direction of available resources. A poster has been created with links to the patient information leaflet which has information on Advance Care Planning and links to next steps and approved templates. Please look for where this poster is displayed in your unit.
For staff that are wanting to access more information, please visit the Advance Care Planning page on the Western Health Intranet.
Have you AICED your patients today?
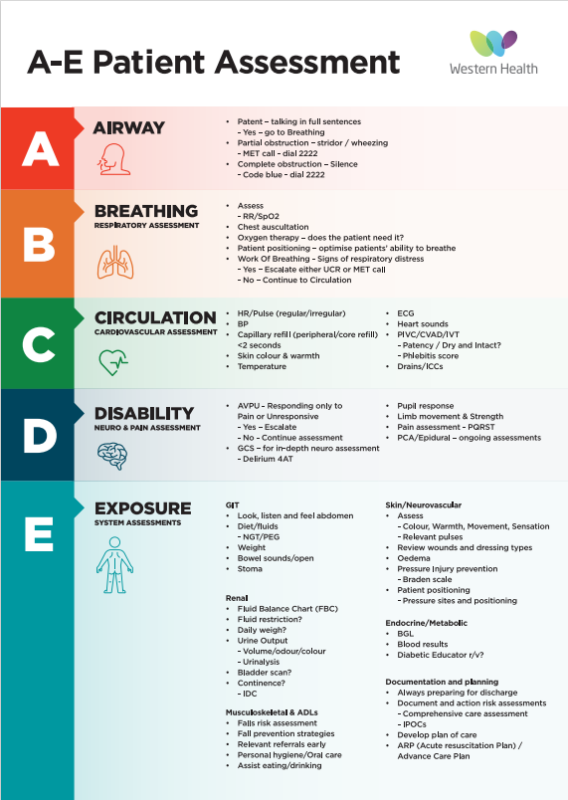
The AICED program commenced during October to support the delivery and documentation of patient care. The initial roll out focuses on adult inpatient areas. It involves a WeLearn package, simulation, face to face sessions on the ward and bedside coaching. Learning will be individualised for your skill and knowledge level.
The program consists of the following:
A – Assessment A-E
- Basic Admission Assessment
- Initial Patient Assessment
I – Identify patient, risks, diagnosis and goals
- Adult Risk Assessment
- Initiate Comprehensive Care IPOC
C – Care Planning and Care Delivery
- Select goals, interventions and orders that reflect assessments
- Review suggested IPOCs and add relevant information to Comprehensive Care IPOC
- Reject suggested IPOCs
- Care delivered to align with IPOCs
E – Evaluate Care
- Document progress using document in plan
- Document variances in nursing shift note
- Review Comprehensive Care IPOC and make changes according to evaluation. Handover.
D – Documentation and Handover
Have you completed?
- Basic admission assessment form
- Initial Patient Assessment
- Adult Risk Assessment
- Comprehensive Care IPOC
- Variances in shift note
- Handover using ISBAR
Have you AICED your patient today?
There is a suite of educational resources. Each week there will be quizzes, crosswords or other activities with a prize each week. There will be small chocolates for completion of learning and a monthly pizza lunch for the best performing ward.
Western Health reaffirms support for First Nations self determination
In the wake of the recent outcome of the First Nations Voice to Parliament Referendum, Western Health acknowledges that this has been a challenging period for many Australians, particularly First Nations people who have long advocated for the Uluru Statement from the Heart and the First Nations Voice to Parliament.
This is a time for unity, and we encourage our whole community to treat each other with respect and integrity.
The Western Health Board of Directors acknowledges the Traditional Custodians of the land on which our sites stand, and we pay our respects to Elders past, present and emerging. We reaffirm our commitment to the healing of country, working towards equity in health outcomes and the ongoing journey of reconciliation.
At Western Health, we are committed to ensuring First Nations people have the right to self-determination during their healthcare journey. We firmly believe in the guiding principle of self-determination, where First Nations people and communities are empowered to own, direct and make decisions in designing their healthcare journey.
This is not the end of the road to reconciliation, a journey that has not been easy for many First Nations people.
It continues to be a constant fight for justice, truth-telling and for self-determination. Western Health pays our respects to those who have fought and those who continue to fight for these rights.
Western Health reaffirms our commitment to working in partnership with our First Nations staff, volunteers, patients, consumers and families to achieve long-lasting improvement and change.
Have your say on the National Nursing Workforce Strategy

Participate in a webinar to inform the National Nursing Workforce Strategy. Webinars will be held from 23 October to 16 November 2023.
A range of webinars are available, sign up to the one that best fits your current experience, role or area of interest. There are also sessions for providers in relevant industries.
Sessions include:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
To register for the webinars please visit National Nursing Workforce Strategy: Webinars | Eventbrite
For more information and other consultation opportunities please visit www.health.gov.au/NNWS
Best Care Week

Best Care Week will run from Wednesday 8 November – Friday 10 November 2023. This year it will focus on the Best Care Framework and how we can deliver Best Care for everyone every time.
The Best Care Governance and Support Team will be running stalls each day providing information on Best Care and are more than happy to answer any questions.
The week will culminate in a webinar and the announcement of our Best Care Awards for 2023. There will be awards for each of the 4 Best Care domains – Person Centered Care, Coordinated Care, Cafe Care and Right Care. Tune into the webinar on Friday 10 November to see who will take home these awards.
Every Week Counts

Western Health is participating in the Every Week Counts National Preterm Birth Prevention Collaborative, which is occurring across Australia. Teams are collaborating regularly and sharing learning as they work towards a shared goal of 20% reduction in preterm and early term birth by 31 March 2024.
Optimal Timing of Birth
It is exciting to see the success being achieved in reducing birth before 39 without medical indications. A range of strategies are being tested in individual services to determine their effectiveness in reducing early birth. These include introduction of a centralised induction of labour booking system, multidisciplinary huddles to review any planned births requested before 39 weeks, and introduction of early timing of birth conversations with women and families to increase awareness of the benefit of birth after 39 weeks. Across the National Collaborative services, so far there has been an 8% reduction in births before 39 weeks.
Cervical length measurement and progesterone prescription
Our team has been working with ultrasound providers and developing local systems to ensure that cervical length is being measured for all women at their mid pregnancy ultrasound scan.
Following the scan, teams are ensuring there is a reliable process to document the scan and that systems are in place to respond in a timely way if there is a shortened cervix, including prescription of progesterone. So far the data shows a 15% improvement across the National Collaborative.
Continuity of Care
One of the most effective strategies in reducing preterm birth, particularly for First Nations women, is providing continuity of care with a known health professional.
The first step for many teams has been collecting data to understand how many women are currently receiving continuity of care and developing local solutions that enable increased access to women with risk factors for early birth.
At Western Health we provide access to Aboriginal lead midwifery continuity of care for First Nations women through our Galinjera program, and we are working hard to extend this program to more First Nations women.
New Mental Health & Wellbeing Centre is now open
The new Sunshine Mental Health and Wellbeing Centre opened last month, and our Acute Mental Health teams have transitioning into this amazing new facility.
Please click on the image right to view a virtual tour, where you will hear from some of our Mental Health and Wellbeing Services team, as well as one of the architects and an arts curator about co-designing a recovery-orientated environment. They represent a much larger group of staff across Western Health and partner organisations who have shown enormous dedication, care and passion to deliver improved mental health and wellbeing services for our communities.
Due to the scale and detail of the build, the video is almost 7 minutes long but it’s well worth a look. The new Sunshine Mental Health and Wellbeing Centre will enable Western Health to provide Best Care to our consumers when they need acute mental health treatment and care.
Further information about the facility and our Mental Health and Wellbeing Services division is available via Westerly.
Changes to Pathology Specimen Collection
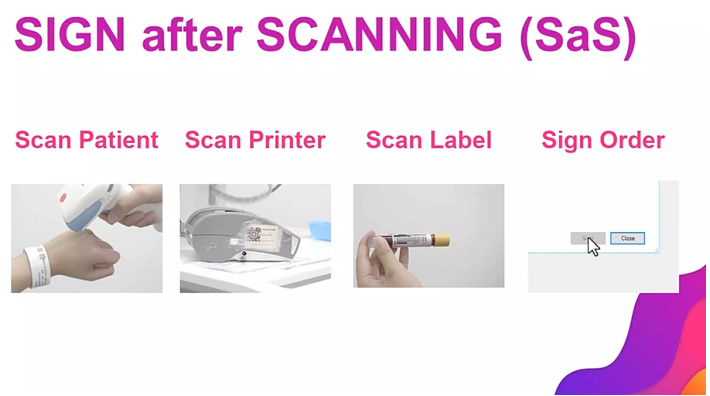
From 13 November 2023, it is essential for staff to sign a pathology specimen in the EMR in order for it to be processed by the labs.
This is consistent with the ‘Sign After Scanning’ workflow currently in effect.
Staff must ensure they:
- Scan the specimen barcode
- Complete the workflow by clicking ‘Sign’ in the EMR to add a date and time stamp to the specimen
Currently when this is not completed, the labs date and time stamp the specimen (with an incorrect date and time).
From this date, the labs will be unable to edit order details, so failure to sign will mean the specimen is not processed.
The Digital Health team will provide support to the labs for one week (13 – 17 November), by phoning clinical areas when an unsigned specimen comes through and reminding staff to complete the workflow.
From 18 November, it will be up to the labs if they wish to phone the clinical area or to not process the specimen, which will result in a rebleed.
To help staff become familiar with this change, a short video for this workflow and helpful Quick Reference Guides are available on the Digital Health information site.
For questions regarding this change, please contact Deputy Chief Nursing & Midwifery Informatics Officer, Barbara Lennon – Barbara.Lennon@wh.org.au
Emerging Research Leader program

Are you a passionate nurse with a thirst for knowledge and a desire to make a difference?
The Australian College of Nursing’s new Emerging Research Leader program is designed to empower nurses like yourself to embark on an exciting research journey.
The 9-month program includes expert led practical workshops, one-on-one mentorship, and self-paced online learning to give you all the tools you need to take your nursing career to new heights.
Participants get the chance to publish research findings as a lead author, all while receiving valuable research grants.
Ready to dive into the world of nursing research? The ACN Foundation is offering fifteen scholarships, each valued at $10,000 for registered nurses to participate in the inaugural intake of the ACN Emerging Research Leader Program.
Apply now – applications close 11:59pm, Sunday 5 November 2023.
Western Health finalists in Victorian Public Healthcare Awards

Two teams from Western Health have been announced as finalists in the Victorian Public Healthcare Awards. This is an outstanding achievement and we extend our congratulations to:
- Finalist Excellence in Values-Based Healthcare – Perioperative and Critical Care Division
- Finalist Excellence in Aboriginal Health and Wellbeing – The Babaneek Booboop Program.
In 2022, our Perioperative and Critical Care Division established the same-day discharge initiative for patients undergoing laparoscopic cholecystectomy and hernia repair surgery. The new approach was inspired by success in other countries and was designed to alleviate the strain on hospital beds following the COVID pandemic. The project has already improved patient access to surgery, reduced length of stay and enhanced patient satisfaction. In one year, more than 300 patients who would have stayed overnight instead left on the same day as their surgery. The initiative showcased the benefits of timely and efficient surgical care while optimising resources and improving patient outcomes.
The Babaneek Booboop Program promotes the health and developmental outcomes of First Nations children in Melbourne’s western suburbs (the City of Melton and Moorabool Shire). Establishing and building on strong networks, the program has supported more than 350 children and their families in their engagement with child health and promoted cultural safety in health. It’s seen more than 97 per cent of participants complete maternal and child health key ages and stages assessments. It’s also led to significant uptake of oral health, audiology, optometry and NDIS referrals. The program is currently funded by the Department of Families, Fairness and Housing through Korin Korin Balit-Djak funding, and is led and managed by Western Health.
Well done to the following program leads and key contributors of these respective programs.
The West Metro Health Service Partnership, of which Western Health is a key partner, was announced as a finalist for the Health Service Partnership of the Year. Since its establishment two years ago, the partnership has built strong connections with more than 280 stakeholders and delivered significant impact through 13 collaborative projects.
Clean your hands, clean your WoW!

Hospitals rely heavily on portable medical equipment, with workstations on wheels (WOWs) being among the most frequently used devices. Consequently, these carts can serve as potential sources of infections if proper precautions are not taken during their use and maintenance.
Maintain a Clutter-Free Environment
Medical carts can quickly become pretty messy if users are not vigilant. It is crucial to ensure that clutter is kept off the WOWs to prevent the risk of infections. It is important to remember that WOWs are not intended for use as procedure trolleys. By keeping them clutter-free, we reduce the surface area available for bacteria and other pathogens to thrive.
Regular Cleaning and Disinfection
Given the pivotal role that WOWs play in our healthcare facilities, they also present a risk of transmitting infections among patients and staff. These machines are susceptible to contamination from the hands of healthcare workers (HCWs). Numerous studies have revealed that both pathogenic and non-pathogenic organisms can persist on WOW surfaces for extended periods. Therefore, it is imperative for healthcare workers to understand the significance of cleaning and disinfecting WOWs. Here are some guidelines for maintaining cleanliness:
- Wipe Down at the Start of Each Shift: The WOW should be wiped down at the beginning of every shift.
- Clean Before Changing Locations: Clean the WOW before moving it to another bed space or patient room.
- Use a Neutral Detergent Wipe: Utilize a neutral detergent wipe that is available on the WOW for cleaning.
- No Personal Belongings: Do not place staff belongings, staff beverages, water bottles, meal trays, or linen on the WOW.
- Gloves Off for Computer Use: Do not wear gloves when operating the WOW computer or computer device.
- Prioritize Hand Hygiene: Perform hand hygiene before and after touching the WOW.
- Hand Hygiene Protocol: Adhere to hand hygiene protocols following interactions with the computer device and before touching the patient (Moment 1).
Managing Patients with Transmission-Based Precautions
In cases where patients require transmission-based precautions (such as respiratory and contact precautions), it is crucial to follow specific guidelines:
- No WOWs in Patient Rooms: WOWs must not be taken into the rooms of patients with transmission-based precautions.
- Avoid Device Use in Patient Rooms: Staff should refrain from using the device in the rooms of patients with transmission-based precautions.
- Proper PPE Removal and Hand Hygiene: Staff should remove all personal protective equipment (PPE) and perform hand hygiene before touching the WOW outside the patients’ room.
By diligently adhering to these guidelines, we can reduce the risk of infections associated with WOWs and ensure the safety of both patients and healthcare workers.
Update on RN prescribing

The Nursing & Midwifery Board of Australia (NMBA) recently closed consultation on the regulation impact statement after receiving over 120 responses to the options and impacts we put forward for a proposed model of designated registered nurse (RN) prescribing.
The proposed model will enable Registered Nurses (RN) with an endorsement for scheduled medicines to prescribe within their level of competence and scope of practice, in partnership with an authorised prescriber such as a medical practitioner or a nurse practitioner. The designated RN prescriber will have authorisation to prescribe medicines that is determined by legislation and will also need to meet the requirements of the NMBA related to the endorsement, and the policies of the jurisdiction, employer or health service.
With overwhelming support for designated RN prescribing, the NMBA will be submitting a decision regulation impact statement with the preferred option to the Office of Impact Assessment and health ministers for review.
Thunderstorm Asthma season

October to December is thunderstorm asthma season in Melbourne. The thunderstorm asthma monitoring, prediction and alert system in Victoria notifies of high-risk events this pollen season, so that people at increased risk – such as those with asthma or hay fever – can take action to avoid exposure to the pollen fragments that can trigger asthma.
Grass pollen season, which typically runs from the start of October until the end of December, brings with it a seasonal increase in asthma and hay fever and the chance of thunderstorm asthma. When large numbers of people develop asthma symptoms over a short period of time, caused by high amounts of grass pollen and a certain type of thunderstorm, it is known as epidemic thunderstorm asthma.
The forecasting system, which will operates each year until 31 December, forecasts three days in advance and provides a low (green), moderate (orange) or high (red) risk forecast across the nine Victorian weather districts. On high-risk thunderstorm asthma risk forecast days, people with asthma or spring hay fever can reduce their risk by avoiding the storms. On these days, at-risk people should go inside, close windows and turn off any air conditioners that bring air and possible pollen fragments in from outside.
Melbourne experienced the world’s largest epidemic thunderstorm asthma event on 21 November 2016, which resulted in 10 tragic deaths and thousands of people developing breathing difficulties in a very short period. Those at risk should check the epidemic thunderstorm asthma risk forecast daily at emergency.vic.gov.au/respond or download the app and set up a watch zone.
Benchmarking Best Care
The latest benchmark reports from the Health Roundtable that go up to June 2023 show how our delivery of Best Care compares to other health services across Australasia.
The latest benchmark reports from the Health Roundtable that go up to June 2023 have recently been released, that show how our delivery of Best Care compares to other health services across Australasia.
Let’s look at how we perform in the area of pressure injuries. The following data looks at Western Health’s rate of Stage III, Stage IV, unspecified and unstageable pressure injuries, and suspected deep tissue injury.
Pressure Injuries:
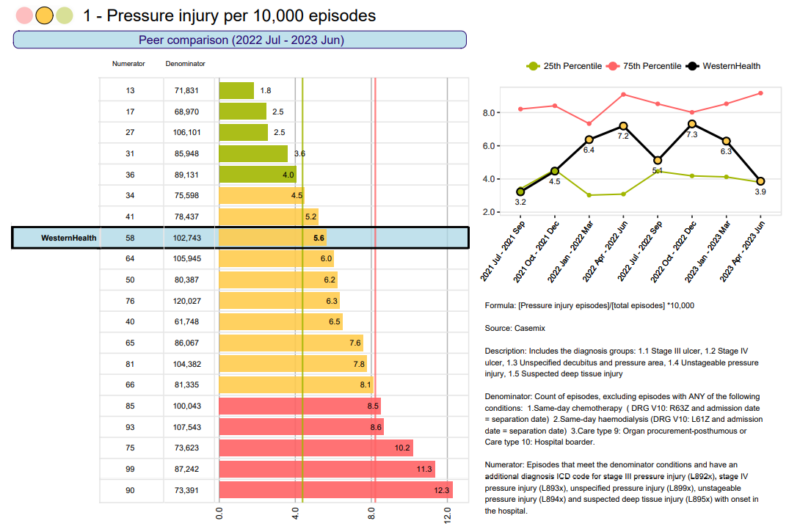
The rate of hospital acquired pressure injuries has dropped for the past 2 quarters, and we are now low amber. This is great improvement – well done!
We remain amber when compared to our peers, however we are nudging green.
New hybrid mattresses will be implemented in
Educational Opportunities

Education and Learning upcoming events:
- 01/11/2023: Stroke Study Day
- 02/11/2023: Deteriorating Patient Study Day
- 02/11/2023: Respiratory Study Day
- 15/11/2023: Heart Failure Study Day
- 21/11/2023: Nutrition Study Day
- 23/11/2023: ALS2 Training
More courses click here: Courses and Inservices (westernhealth.org.au)
Course Enrolment/Inquiries:
- WeLearn Helpdesk Email: welearn@wh.org.au
- WeLearn Enrolment link: welearn@wh.org.au
Emerging Evidence
The Western Health Library Service is a great source for locating the latest nursing and midwifery related evidence-based practice and research.
Latest articles of interest:
- Equitable access to COVID-19 diagnostics: factors associated with the uptake of rapid antigen testing in Victoria, Australia, January – February 2022. BMC Public Health. 2023: November. Full Text Western Health Author
- Family experiences and perceptions of intensive care unit care and communication during the COVID-19 pandemic…Australian and New Zealand Intensive Care Society/Australian College of Critical Care Nurses (ANZICS/ACCCN) Intensive Care Annual Scientific Meeting, March 29-31, 2023, Adelaide, South Australia. Australian Critical Care. 2023: Supplement 1. Request Article Western Health Author
- Impact of the COVID-19 pandemic on Australian community health service staff’s occupational and personal lives: a longitudinal study. Australian Journal of Primary Health. 2023: October. Full Text Western Health Author
- Staff experiences, perceptions of care and communication in ICU during the COVID-19 pandemic in Australia…Australian and New Zealand Intensive Care Society/Australian College of Critical Care Nurses (ANZICS/ACCCN) Intensive Care Annual Scientific Meeting, March 29-31, 2023, Adelaide, South Australia. Australian Critical Care. 2023: Supplement 1. Request Article Western Health Author
New Nursing/Midwifery eBooks
- ECG Interpretation Made Incredibly Easy! 7th ed. Wolters Kluwer Medical, 2020. (Ovid eBook Guide)Offering expert direction, this freshly updated, fully illustrated guide is packed with images and learning aids that support your understanding and retention in obtaining and interpreting rhythm strips. Recognize and treat a wide variety of arrhythmias with this vital text — an ideal study aid and friendly on-the-unit support for both students and practicing nurses. Get skilled and confident in rhythm strip interpretation and treating arrhythmias. NEW and updated content in a quick-read, bulleted format that makes it easy to spot important points at a glance. Dozens of colourful diagrams and illustrations that outline core terms and concepts, with easy-to-retain definitions of key terms.
- Clinical Practice Guidelines for Midwifery & Women’s Health. 6th ed. Jones & Bartlett Learning, 2022. (ProQuest eBook Central Guide)Clinical Practice Guidelines for Midwifery & Women’s Health, Sixth Edition remains an accessible and easy-to-use quick reference guide for midwives and women’s healthcare providers. Thoroughly updated and revised to reflect the changing clinical environment, it offers current evidence-based recommendations, updated approaches, and opportunities for midwifery leadership in every practice setting. The Sixth Edition features new information on diversity and inclusion, sexual health, opioid disorder and substance-exposed newborns, care for the individual who is transitioning and after transition, and more timely and relevant topics.
Clinical Practice Guidelines
The library has created a web page collating international and Australian Clinical Guideline websites. CPGs bring together the best available research evidence and provide benchmarks for best-practice. The page includes tips for finding guidelines on databases.
Accessing the Library at Work:
All eligible staff can access electronic library resources from any networked PC or device connected to Wi-Fi network without the need to login.
Accessing the Library Remotely (offsite access):
- When accessing electronic resources through the library website from offsite you will automatically be asked to enter your library membership number and surname.
- Library Membership is free and can be completed online. Please email the library if you experience issues when registering (e.g. error messages).
For more information please contact the Western Health library team.


