Edition 79: April 2024
-
Helpful contacts
Employee Assistance Program: 1800 099 444
Nurse & Midwife Support: 1800 667 877
Nurse & Midwife Health Program: 03 9415 7551 or 1800 888 236
-
Upcoming dates
April 2024
1 Mental Health & Wellbeing Legislation regarding restrictive practice in EDs and UCCs implemented
7 World Health Day
12 Inspire Award nominations close
15 Nursing Trailblazers applications close
16 Advancing Frontline Leadership program (Group 1)
20 ACN Nursing & Health Expo – Melbourne Convention & Exhibition Centre
23 Advancing Frontline Leadership (Group 1)
24 World Immunisation Week commences
25 ANZAC Day
26 Joy Turner Memorial Scholarship applications closeCheck out Events for more details.
-
Nursing & Midwifery Executive
Adjunct Professor Shane Crowe
Executive Director of Nursing & Midwifery
Phone: 8345 1463
Email: shane.crowe@wh.org.auDoug Mill
Director of Nursing & Midwifery
Division: Western@Home
Phone: 0400 807 938
Email: douglas.mill@wh.orh.auAdjunct Associate Professor Jo Mapes
Deputy Executive Director of Nursing & Midwifery
Division: Education & Learning
Phone: 0423 302 337
Email: joanne.mapes@wh.org.auKylee Ross
Director of Nursing & Midwifery Informatics (CNMIO)
Division: Digital Health
Phone: 0409 555 384
Email: kylee.ross@wh.org.auLena Pejcinovski
Director of Nursing, DPFC
Division: Custodial Health
Phone: 0422 818 187
Email: lena.pejcinovski@wh.org.auProfessor Linda Sweet
Chair of Midwifery, Deakin University/Western Health
Phone: 8395 1178
Email: linda.sweet@wh.org.auLisa Gatzonis
Director of Nursing & Midwifery Workforce
Phone: 0466 943 769
Email: lisa.gatzonis@wh.org.auMichelle Read
Director of Nursing & Midwifery
Division: Surgery, Endoscopy & Anaesthesia Services
Phone: 0478 260 237
Email: michelle.read@wh.org.auMonique Sammut
Director of Nursing & Midwifery, Sunbury
Divisions: Aged, General Medicine & Subacute Services and WPHU
Phone: 0412 769 423
Email: monique.sammut@wh.org.auNicole Davies
Director of Nursing & Midwifery, Williamstown
Divisions: Emergency Medicine & Intensive Care Services and Access & Patient Flow
Phone: 0435 656 190
Email: nicole.davies@wh.org.auRobyn Peel
Director of Education & Learning
Phone: 0468 608 141
Email: robyn.peel@wh.org.auProfessor Rochelle Wynne
Chair of Nursing, Deakin University/Western Health
Phone: 8395 8163
Email: rochelle.wynne@wh.org.auRohan Vaughan
Director of Nursing & Midwifery, Melton
Divisions: Clinical Support & Specialist Clinics and Drug Health Services
Phone: 0434 365 769
Email: rohan.vaughan@wh.org.auRyan Dube
Director of Nursing
Division: Mental Health & Wellbeing
Phone: 0420 228 035
Email: ryan.dube@wh.org.auAdjunct Professor Tanya Farrell
Deputy Executive Director of Nursing & Midwifery/Director of Maternity Services
Division: Women’s & Children’s
Phone: 0468 830 755
Email: tanya.farrell@wh.org.auVal Dibella
Director of Nursing & Midwifery
Division: Cancer Services, Cardiology & Specialist Medicine
Phone: 0466 489 687
Email: val.dibella@wh.org.auWendy Giddings
Director of Nursing & Midwifery, Bacchus Marsh
Divisions: Western@Home and Integrated Community Health Services
Phone: 0458 603 897
Email: wendy.giddings@wh.org.auAdjunct Associate Professor Wendy Watson
Deputy Executive Director of Nursing & Midwifery
Division: Best Care Governance & Support
Phone: 0478 305 046
Email: wendy.watson@wh.org.au
From Shane

One of the best things about working at Western Health is that we are surrounded by inspirational people that really excel at what they do, and who go above and beyond to deliver or support Best Care. We all know someone that inspires us and who really makes a huge difference. These people demonstrate a deep commitment and sense of purpose, and usually do not work here for accolades or glory – however, isn’t it wonderful when we can recognise and celebrate them! Here’s your chance. Nominations for our annual Inspire Awards are currently open and are an excellent opportunity to recognise our very own super-stars and let them know just how much they are appreciated. I encourage you take some time to nominate that special person, people or team prior to 12 April, ahead of the ceremony later this year.
Unfortunately, occupational violence and aggression (OVA) continues to be a significant risk for healthcare professionals. We take this risk extremely seriously at Western Health, as all of our people deserve to be safe at work. Over the past years we have made some impressive inroads on decreasing the number and severity of OVA incidents across our hospitals, through the Predict Prevent Priority: Safety campaign and tools and Safewards. I’m excited that after a couple of years of development, our next important initiative is finally here. Our innovative new ‘Reframe your response’ virtual reality training package simulates real-world scenarios in a healthcare setting to demonstrate how self-awareness and emotional regulation during difficult situations can shape and influence a safe and effective outcome. Virtual reality is demonstrated to achieve enhanced focused learning, helping learners to get more out of the training and have better outcomes. This new package has been custom built for Western Health, and I encourage you to book in and experience it for yourself!
Towards the end of March we were notified that Western Health received our accreditation for 3 years. This is the first time that we have undertaken the new short-notice accreditation survey since it was introduced in 2023, and I was so immensely proud of how Best Care at Western Health was demonstrated to the 12 surveyors. My sincere thanks to everyone for your tireless dedication in continually delivering or supporting the provision of Best Care to our community every day. We now have 6 months where we cannot be surveyed again, however our next short-notice accreditation survey can be any time after that! I am confident that the systems and processes we have in place will ensure that we are always ‘accreditation-ready’ going forward.
Our Employee-centered Rostering steering committee has begun to meet and is busy getting everything finalised ahead of the upcoming implementation. The draft guideline will be approved and published over the coming couple of weeks, together with educational material and a communications plan. The implementation will commence in our pilot areas, which include all our Joan Kirner Women’s & Children’s maternity wards, Ward 1A, Ward 3B and Ward 3F. This initial implementation will give us a chance to finesse things prior to a wider implementation across all our wards and departments over the coming months. This incredibly important project aims to support our nurses and midwives to balance their lives inside and outside of work through enhanced flexibility, enhancing fairness and decreasing fatigue by optimising rosters and break periods.
Changes to the care and governance requirements under the Mental Health & Wellbeing Act 2024 were implemented in our Emergency Departments and Urgent Care Centres on 1 April 2024, whereby the use of all restrictive interventions (including bodily restraint, chemical restraint and seclusion) for consumers receiving care under that Act are reportable to the Chief Psychiatrist.
If you are a point-of-care nurse or midwife who has played an active role leading a quality improvement initiative within your ward or department, I encourage you to apply for a Joy Turner Memorial Scholarship. Ther are 5 scholarships of up to $2,000 to support you to attend any health-related conference of your choosing.
The ANMF held a report back meeting on 21 March 2024 regarding the status of the nurses and midwives enterprise agreement negotiations. The offer made by the Victorian Government was presented, and whilst there was support for the progress made on non-cost items, a Resolution was made at the meeting to reject the offer and make an application for a protected industrial action ballot order in the Fair Work Commission. In the meantime, when an application for protected industrial action is made, the Fair Work Commission insists on compulsory conciliation between the parties to discuss the impact of the proposed industrial action. Any industrial action cannot occur until after the current enterprise agreement expires on 30 April 2024. I will continue to keep you all informed as things progress.
Finally, my congratulations to Wendy Watson who has recently be recognised by Deakin University by being awarded an Adjunct Associate Professor title. Well done Wendy!
Shane Crowe
Executive Director, Nursing & Midwifery
This month we are focusing on...
 Standard 7: Blood Management
Standard 7: Blood Management
An ongoing Standard of the Month program has been introduced to support us to remain ‘accreditation ready’ at all times. This involves a focus on one Standard per month, with communications and walkarounds to help staff be aware of how Best Care at Western Health reflects this Standard, to ask staff possible Surveyor questions and answers, and to walk in a Surveyor’s shoes to see what our practice at Western Health looks like.
We are excited that NSQHS Standard 7: Blood Management is to be the focus of April’s Standard of the month. This will run from Tuesday 2 April to Friday 26 April. Look out for friendly Fab 5 Team Members, Best Care Co-ordinators, and other staff who will visit clinical areas/departments to discuss Blood Management with you.
Click here to view a calendar of Blood Management Standard of the Month activity.
Our aim is to have every clinical department/service across Western Health visited within the month. Click here to access the NSQHS Standard 7 Walkaround template that includes Q&As plus a checklist of ‘what can you see’. This template can be used at any time by staff to keep Accreditation Ready for NSQHS Std Accreditation Survey.
To get up-to-date with accreditation readiness and Blood Management, read the NSQHS Standard 7: Blood Management Bulletin. An ‘at a glance’ one pager on the Standard is also available and will be distributed on walkarounds.
Registration Renewal time

The annual renewal of nurses’ and midwives’ registration lets the public and your colleagues know that you’re still safe to practise.
To avoid a late fee renew online before 31 May 2024. All nurses and midwives needing to have renewed their registration prior to 30 June 2024 to allow them to continue to practise.
Western Health does not employ anyone into any nursing or midwifery position without an active registration for any period.
Payment:
To ensure quick and effective renewal, nurses and midwives and encouraged to renew online.
Renewal fees can be paid by credit/debit card. If you do not have a credit/debit card you can purchase a pre-paid debit card from various retail outlets for a nominal fee.
Non-practicing registration:
Every year Western Health has a large number of nurses and midwives go on some extended leave. Often this is for something like maternity leave or long service leave, where they fully intend to return to work following their leave.
Occasionally some of our nurses or midwives have fallen into the trap of applying for non-practicing registration during their leave, which has impaired their ease of returning to work.
The Nursing and Midwifery Board of Australia (NMBA) regulates the practice of nursing and midwifery in Australia, and one of its key roles is to protect the public. The NMBA does this by developing registration standards, professional codes, guidelines and standards for practice which together establish the requirements for the professional and safe practice of nurses and midwives in Australia.
The types of registration available to nurses and midwives who apply to the NMBA to be registered include general registration, provisional registration, student registration and non-practising registration.
All of our active nurses and midwives are on the general register. Non-practising registration is a type of registration that is suitable for an individual who chooses to stop all nursing and/or midwifery practice but wishes – for personal rather than professional reasons – to retain a
protected nursing and/or midwifery title. Often this is a nurse or midwife who:
- has retired from nursing or midwifery practice
- is experiencing a period of prolonged illness, or
- is intending to take a long period of absence from practice.
Nurses and midwives wishing to take a period of leave (i.e. maternity leave) who are intending to return to work are advised to remain on the general register. Please note however that you must be able to maintain your CPD and recency of practice requirements.
Any nurse or midwife that transitions to non-practising registration needs to go though a process to be able to practise again. That includes lodging an application form (AGNP-40) for general registration and meet all the requirements of the following NMBA registration standards:
- criminal history
- professional indemnity insurance arrangements, and
- recency of practice.
If you the nurses or midwife does not meet the recency of practice registration standard requirement, a re-entry to practice requirement will apply.
Tips and information:
Read the renewal FAQs on the Ahpra website for helpful tips and more information on what you need to do to renew.
If you have difficulty renewing your registration online or you have a query about your registration, please contact Aphra by making a web enquiry or by calling 1300 419 495.
Awesome Accreditation outcome

Western Health has been formally awarded 3 years accreditation by the Australian Council of Healthcare Standards and we have received our final reports.
This fantastic result is based on the findings from:
- The accreditation survey held during the week of 4-8 December 2023, where 12 surveyors from across Australia intensively assessed Western Health against the eight National Safety and Quality Health Service (NSQHS) Standards.
- The accreditation final assessment where 2 surveyors visited our sites on 14 March to review the two areas identified in December as requiring some improvement.
The commendations received from surveyors throughout our accreditation journey included:
- There was high praise from the surveyors about the standard of care, commitment to being person-centred, our culture of respect and teamwork and involvement and empowerment of consumers in their care.
- The surveyors commented on how it was apparent that innovation is in Western Health’s DNA, and they were unanimous in their praise for our people.
- The lead surveyor commented that they spoke to a large number of patients and consumers throughout the week, and every single one of them had positive things to say about our people and the care that they were receiving – which she said is unusual.
- All elements of the care that we provide to our patients, women and consumers were highly praised, and it was evident that it was actively being practised at the point-of-care.
- There was noteworthy acclaim from the surveyors about the considerable amount of work undertaken to improve both medical credentialing and the reporting of our learning requirements during the final assessment.
Formal notification with the NSQHS Standards Assessment Reports will be shared with staff once received.
Every single Western Health employee, volunteer and consumer advisor should feel immensely proud of this achievement – your commitment to continually improving is inspiring. My sincere thanks to everyone for your tireless dedication in continually delivering or supporting the provision of Best Care to our community every day.
Changes to restrictive intervention requirements in Western Health EDs and UCCs

Victoria’s new Mental Health and Wellbeing Act 2022 (MHWA) commenced on 1 September 2023.
The MHWA includes obligations and reporting requirements for the regulation of restrictive interventions in designated mental health services. Western Health became a designated mental health service on 1 July 2023 and so these changes apply to us.
What’s new?
From 1 April 2024, changes to clinical practice and governance will come into effect in all of Western Health’s Emergency Departments (EDs) and Urgent Care Centres (UCCs) in relation to restrictive interventions.
Under the MHWA, the use of all restrictive interventions – bodily restraint, chemical restraint and seclusion – on people receiving a mental health and wellbeing service is reportable to the Chief Psychiatrist. This includes all voluntary consumers receiving a mental health and wellbeing service.
What does this mean for all Divisions, programs and sites under the governance of Western Health?
As a designed Mental Health Service, Western Health is required to:
- Implement the provisions set out in the MHWA and apply these to ED and UCC settings from 1 April,
- Understand, by 1 April, mandatory reporting requirements and the Chief Psychiatrist’s expectations of best practice when using restrictive interventions outlined in the Chief Psychiatrist Guideline on Restrictive Interventions (advance final copy),
- Determine when a person is receiving a mental health and wellbeing service and apply the requirements of the MHWA accordingly in all settings where care is provided by Western Health,
- Comply with and give proper consideration to the mental health and wellbeing principles and the decision making principles set out in the MHWA, to guide staff in upholding the dignity and autonomy of people living with mental illness or psychological distress,
- Accurately complete all documentation to ensure authorisation, documentation and reporting requirements are legally compliant.
What supports are in place at Western Health?
A comprehensive education program for staff working in EDs and UCCs, alongside the Mental Health & Wellbeing Services is raising awareness of legislative obligations under the MHWA. Further education in EDs and UCCs can be arranged through:
- Pallavi Pathak: Clinical Nurse Educator Pallavi.Pathak@wh.org.au
- Leslie Mbatia: Clinical Nurse Educator Leslie.Mbatia@wh.org.au
WeLearn Modules
Western Health clinical workforce are encouraged to complete existing MHWA Modules on WeLearn. Module 6 (new) is now available for all staff working in EDs, UCCs, MHWS inpatient units and all inpatient wards.
Module 6 covers protections of the MHWA for the use of restrictive practices; definition of the forms of restraint intervention, monitoring and recording obligations and new reporting requirements.
A flowchart to outline the authorisation, reporting and monitoring of Restrictive Interventions and can be accessed via this link.
Mental Health and Wellbeing Act 2022 Q&A email address
Mental Health and Wellbeing Act 2022 questions can be sent to MHWA@wh.org.au. Emails will be responded to within 48 hrs Mon- Fri. Urgent queries should be directed to your manager, senior medical officer or the Emergency Mental Health team.
Department of Health and Office of the Chief Psychiatrist Readiness Resources
The Chief Psychiatrist’s final guidelines, fact sheets and flow charts can be downloaded from:
Recorded information sessions are also available:
New Footscray Hospital clinical move planning underway

Clinical move planning is essential to ensure the safety of patients, maintain the quality and continuity of health services, comply with regulations, and facilitate a seamless transition for both staff and patients to the New Footscray Hospital (NFH).
To inform the clinical move plan, a patient audit of the Footscray Hospital clinical areas must be carried out to determine:
- the likely numbers of patients to be transferred
- number of days required for the clinical move
- the complexity of patients and care/transfer requirements including transfer team resourcing and NEPT/Ambulance Victoria requirements
The audit will be undertaken by the current Footscray Hospital inpatient wards and Emergency Department/Short Stay Unit in 2 x 2-week blocks commencing March and finishing May 2024 (excluding school holiday period).
NFH Project Managers will work with NUMs (or Nurse-in-Charge) during audit days, scheduling walk arounds and providing support as required between 9:30 AM to 10:30 AM to ensure the seamless collection of data. Patient information will be pre-filled by NFH Project Managers where possible to minimise impact on nursing staff.
The audit will also assist managers in becoming familiar with their new units and in commencing planning in ensuring patients are transferred to the most appropriate location within the new NFH.
Enterprise Agreement update

The Log of Claims from unions (ANMF, HWU and HACSU) and employers, represented by the Victorian Hospitals’ Industrial Association (VHIA) have been the subject of ongoing negotiations between the parties since October 2023.
Meetings have been occurring at least two days a week, where the parties have been working through both employee and employer claims and in many cases the proposed wording of draft clauses has been negotiated to ensure that changes to the enterprise agreement would work effectively and not cause unintended consequences. Negotiations between the parties are overseen by the Department of Health, who represent the State Government and have to support any additional costs if they are included in the enterprise agreement.
On 1 March 2024, the ANMF wrote to the Victorian Government seeking a comprehensive response to all of the union’s claims, and on 19 March 2024 a State Government approved response and offer was provided by VHIA. The offer included a 4-year agreement, a 3% per annum wage increase, a pro rata $1,525 per EFT lump sum payment and agreement to a number of no-cost items.
The ANMF held a report back meeting to update its’ members on the progress of the EBA negotiations on 21 March 2024. Western Health worked actively to ensure that as many of our nurses and midwives that wanted to attend this meeting were able to do so.
Outcome of ANMF enterprise agreement feedback meeting
Whilst there was support for the progress made on non-cost EBA items, a Resolution was made at the ANMF meeting to:
- reject the offer,
- make an application for a protected industrial action ballot order in the Fair Work Commission.
When an application for protected industrial action is made, the Fair Work Commission insists on compulsory conciliation between the parties to discuss the impact of the proposed industrial action.
ANMF will then likely ask its members to vote of the protected industrial action, and then hold a meeting after the declaration of the protected industrial action ballot to advise their members on next steps. Any industrial action cannot occur until after the current enterprise agreement expires on 30 April 2024.
In the meantime, the parties will continue to meet to work through unresolved items. Western Health is hopeful that further progress will be made in these meetings.
Keeping informed
Western Health will continue to provide regular updates on the outcomes of the bargaining process and how the new enterprise agreements for 2024-2028 are progressing.
Unions will also provide information to their members through regular publications, notices and report-back meetings.
Any queries or concerns can be discussed confidentially with the relevant Divisional Director of Nursing & Midwifery, Deputy Executive Director of Nursing & Midwifery or People & Culture Business Partner.
Reframe your response - new virtual reality OVA training

‘Reframe your response’ is a new training package that uses virtual reality to simulate real-world scenarios in a healthcare setting. Based on the premise that ‘where there is an event, you have a response to that event, that creates an outcome’ the aim of the training is to demonstrate how self-awareness and emotional regulation during difficult situations can shape and influence an outcome. Reframe Your Response is an educational workshop developed to increase healthcare staff members’ skills in preventing and de-escalating behaviours of concern in the workplace.
The program combines educational content with experiential learning, and the production of individualised plans for staff to increase their awareness and approaches to manage stress over time.

Wearing VR headsets, training participants view the scenarios from the perspective of the patient in order to better understand and empathise with their experience of being in hospital. The second scenario is a Ward Scene, in which the user experiences a nurse’s perspective of interacting with a stressed visitor (a family member of an acutely unwell older woman). In the latter scenario, the user is presented with various decision points that impact the outcome of the interaction.
Using virtual reality’s capacity to better connect people emotionally with training material, the immersive Reframe training helps increase the confidence, compassion and safety of participants.
The new Virtual Reality training was introduced on 27 March 2024 and is really amazing and innovative – and shown to have a positive impact on staff learning.
Links to the registration below:
- Staff from High Risk OVA areas (Emergency Departments, Ward GC, Ward 2A, Ward 3E)
- Staff from other areas
Please note that staff from Mental Health & Wellbeing undertake a different bespoke OVA education program.
Nominate our Inspiring nurses and midwives

The Western Health Inspire Awards recognise employees and volunteers, individuals and teams, whose actions inspire others to live our values. They offer you another way of saying thank you to someone who has made a difference to your day or to the experience of patients or others.
We would like to encourage patients, visitors, employees and volunteers to help us promote our values and a positive workplace at Western Health by nominating individuals or teams who are making a difference for an award.
The Inspire Awards recognises those who foster a positive workplace at Western Health by demonstrating our values through:
- Compassion – consistently acting with empathy and integrity and improving the experience of patients.
- Accountability – empowering our staff to serve our community, taking responsibility for standards of care or service, being positive and productive and using resources responsibly.
- Respect – for the rights, beliefs and choice of every individual, communicating respectfully in all situations and recognising and respecting diversity.
- Excellence – inspiring and motivating, innovation and achievement, demonstrating high standards of work, helping others learn and improve and working well with others.
- Safety – prioritising safety as an essential part of everyday practice and looking out for the safety of others.
How To Nominate:
All you have to do is to tell us why your nominated person or team deserves a thank you and we will enter them into the next award process. To ensure your nomination is successful:
- Explain what they did which has made a difference to your experience or the experience of others. Include examples and provide as much detail as you can.
- Please make sure that you address the following criteria. How did they contribute to fostering a positive workplace? How did they demonstrate the values of Compassion, Accountability, Respect, Excellence and Safety?
Nominations can be submitted via Online Nomination Form or the Nomination form (Word version) and close on 12 April 2024. Award winners will be announced at a live streamed presentation event annually.
Joy Turner Memorial Scholarships now open

Joy Turner was a Director of Nursing & Midwifery at Western Health from 2014 until 2020, and sadly passed away in March 2023. During her time at Western Health she made long-lasting impacts through her significant leadership to the nursing workforce. She was a strong advocate for our patients and staff, and mentored many people to support their development.
Western Health offers the Joy Turner Memorial Scholarship Program on an annual basis to support frontline nurses/midwives who are involved in local quality improvement initiatives, to attend a health-related conference. The scholarship of up to $2,000 is awarded annually to five point-of-care nurses/midwives to reduce the cost burden related to attending a health-related conference.
Western Health recognises our bedside nurses and midwives are critical members of the healthcare team, and their involvement in quality improvement initiatives is essential to improve patient outcomes, reduce errors, and enhance overall patient experience. Nurses and midwives are often in the best position to identify areas that need improvement and develop innovative solutions. Nurse/midwife-led quality improvement initiatives have been proven to increase patient satisfaction, reduce healthcare costs, and improve the overall quality of care.
The involvement of bedside nurses and midwives in quality improvement initiatives is crucial to drive meaningful change and continuously improve patient outcomes.
Eligibility:
The Joy Turner Memorial Scholarship Program is open to all point-of-care nurses/midwives employed at Western Health who have played an active role leading a quality improvement initiative within their ward.
Applicants must provide evidence of the quality improvement initiative, together with a letter of recommendation from their ward manager.
Scholarship Award:
Every year, a scholarship will be awarded (up to $2,000 each) to five point-of-care nurses/midwives to reduce the cost burden related to attending a health-related conference.
The funds will be reimbursed directly to the scholarship recipient once confirmation of conference registration and payment has been received. The scholarship recipient will be responsible for making their own arrangements to attend the conference.
Application process:
Please complete the application form and return it and supporting documentation to NursingMidwiferyLeadershipPrograms@wh.org.au. Applications for will close on Friday 26 April 2024.
Nursing Trailblazer Award nominations now open

The Health Minister’s Award for Nursing Trailblazers (Trailblazers Award) recognises nurse leaders and innovators who lead the way to transform our health and aged care systems by impacting costs, improving quality of care and enhancing consumer satisfaction. The award acknowledges nurse-led innovations and models of care which significantly improve health outcomes for the Australian community through evidence-based processes.
Founded in 2019, the Trailblazers Award is administered by the Australian College of Nursing (ACN). The award is designed to acknowledge that nursing has the solutions to many of the problems that plague the Australian health and aged care systems. This prestigious award is bestowed upon an innovative and outstanding nurse who has demonstrated leadership to bring new thinking to a wide range of health care challenges.
The ACN facilitates the nomination and selection process in line with the following selection criteria:
- Significant contribution to the nursing profession and better health outcomes of Australian community
- Innovative work of nurses and the holistic and integrated philosophy underlying nursing care
- Demonstrated innovative intervention or excellent model of care that resolved a problem in the delivery of health care or an unmet health need of a population.
Nominations for the 2024 Health Minister’s Award for Nursing Trailblazers are now open. To nominate yourself or an innovative colleague please complete the nomination form. Nominations will close on Monday 15 April 2024.
National Maternity Workforce Review Project update

The National Maternity Workforce Review Project commenced in January 2024, with the aim of understanding existing maternity strategies and workforce plans, key models of care and the workforce delivering them across Australia.
Throughout the Review Project, the Project Steering Group facilitated several targeted consultation activities, including:
- a national online survey in February
- a series of online focus groups for stakeholders representing priority groups
- a national online open forum held during March.
Western Health has participated in each phase of this project and has shared our own Nursing & Midwifery Workforce Plan to help inform this important work.
The project has now concluded its engagement and consultation process and has moved into analysing all collected data and compiling a report. The report will include identifying the current strategies and workforce plans across jurisdictions, workforce groups delivering maternity care, and the future risks of the maternity service workforce.
The final report will be submitted to the Health Workforce Taskforce (HWT) for review and consideration in April. It is expected to be distributed more widely once approved by the HWT.
Congrats to these notable appointments

Assistant Chief Nursing and Midwifery Informatics Officer
Congratulations to Barbara Lennon who was recently appointed to the position of Assistant Chief Nursing and Midwifery Informatics Officer (Nursing and Midwifery Informatics Advisor) after a highly competitive recruitment process.
With an illustrious journey spanning over 25 years, Barbara brings a wealth of experience and expertise to her new role. Barbara commenced her journey with Western Health in 2017, assuming the pivotal role of EMR Learning and Development Manager. Her dedication and passion for advancing healthcare through technology were evident from the outset, as she seamlessly integrated her extensive knowledge gained from her years as a nurse in ICU.
Throughout her tenure, Barbara has remained at the forefront of EMR innovation, transitioning from an end user to a key figure in configuration and education. Her hands-on experience, coupled with her unwavering commitment to excellence, has been instrumental in shaping the digital landscape.
In July 2023, Barbara embarked on a new chapter as Acting Nursing and Midwifery Informatics Advisor (Assistant Chief Nursing and Midwifery Informatics Officer), where she played a pivotal role in steering the course of EMR Phase 2.1 optimisation and other critical Digital Health initiatives. Her visionary leadership and strategic acumen have been invaluable assets in driving forward our digital transformation agenda.
We are confident that Barbara’s appointment will further elevate Western Health’s digital capabilities and propel us towards new heights of innovation and excellence. Congratulations Barbara on this well-deserved achievement!

Education Manager – Interprofessional Education Lead
Emma Thaus has been appointed to the Education Manager – Interprofessional Education lead role here at Western Health. Emma has worked in education for a number of years as a Clinical Nurse Educator, undergraduate educator and undergraduate coordinator. She has achieved amazing things in the undergraduate space and adapted well to COVID maintaining clinical placements and continuing to deliver great experiences for the students.
Most recently Emma has been involved in a multidisciplinary project around NWAU funding and documentation and has been instrumental in this project, already delivering good outcomes. Emma has a Masters in Education and has also worked in the tertiary sector. She brings a strong educational and clinical background to this role. I am sure you will all join me in congratulating Emma and supporting her in this new role.
Deputy Director, Nursing & Midwifery Workforce
We’re pleased to announce the appointment of Rohan Kan as Deputy Director of Nursing and Midwifery Workforce after a highly competitive recruitment process.
Rohan brings a wealth of nursing and leadership experience having worked as a Nurse Manager, Critical Care Educator, Assistant Director of Nursing and Director (Pandemic Response) with Tasmanian Health Service.
Having recently worked in centralised staffing roles, he brings a sound knowledge of supporting managers with workforce planning, recruitment and operational leadership of supplementary staffing and allocations.
Rohan will commence in the role on Tuesday 2 April 2024.
CPO Environmental Risk Factors
The transmission of highly resistant pathogens such as Carbapenemase-producing organisms (CPO), other multi-resistant organisms, Clostridioides difficile and norovirus can have significant impacts for the patient and on the healthcare facility in its ability to provide patient services.
CPOs are highly resistant bacteria found in the human bowel, including Klebsiella, E. coli, Acinetobacter, and Pseudomonas. They have previously been referred to as CRE or CPE but now are collectively known as CPO. Some CPOs have acquired genes that make them resistant to antibiotics, including carbapenems. When people get serious infections from CPO, there can be limited antibiotic treatment with associated high mortality rates.
Stringent hand hygiene, equipment cleaning and environment cleaning are the cornerstone for the prevention of disease transmission and protection of patients in healthcare settings.
The use of WoW’s and LoW’s can be a source of environmental transmission to the patient and the environment. A Victorian public hospital identified the introduction of mobile computer stations as one of the key factors associated with increased CPO cases and transmission of CPO in their facilities stemming from one clinical area. The nature of WoWs is that they are highly mobile, go from patient to patient and across areas, and are used for other purposes than just as a computer station, which then increases transmission risk to patients.
WOW’s are a high use piece of communal equipment, entering multiple patient areas and handled by numerous staff members. They are not a part of the patient zone so hand hygiene and cleaning between contact with the patient zone (inside the bedside curtain or room) and the WOW is essential. Pathogens can have significant survival times in the environment – ranging from hours up to over 48 months (depending on the pathogen)!
Current Concerns
Alertness level: High, with a moderate to high level of concern. Sunshine Hospital has 4 declared Victorian Transmission Risk Areas (TRA) which means Sunshine patients admitted elsewhere across Victoria are screened and isolated by other organisations with follow up to Western Health’s Infection Prevention team for 12 months. The first transmission triggered 1,600 contacts for tracing and following up including post-discharge, one of the more recent cases has had 1,000 contacts. This volume of contacts puts significant pressure on the organisation for single rooms, striction isolation, additional cleaning, and increased infectious risk alerts.
Sunshine Hospital currently has 3 different strains of CPO with 2 of these unique to Sunshine that have not been identified elsewhere in Victoria and are imported from overseas healthcare treatments with ongoing unidentified chains of transmission to other patients. Patients are also highly mobile within wards, across wards and across our hospitals which increases risk of transmission. There has been an increase in cases with international travel post borders opening.
Review of WoWs and LoWs at Sunshine Hospital: Sunshine Infection Prevention team have undertaken audits of WoWs and LoWs both ward based and medical based after identifying several practice issues that could be contributing to transmission with wards and across wards. There has been noted improvement in the cleanliness and usage of WoWs from January to current. The common issues observed are:
- Lack of Clinell Disinfectant wipes and alcohol hand rubs on the WoWs,
- Lack of cleanliness of the WoWs surfaces,
- Sterile equipment stored on surfaces, in empty Clinell holders
- IV infusions and IV medication on contaminated, unclean surfaces
- Medicine cups stored in contaminated mouse holders, spoons, jelly on WoWs which increases risk of patient ingestion of such pathogens directly into the patient’s mouth from such contaminated surfaces.
- Occasional coffee cups and several water bottles of staff
- Patient equipment, shared equipment used on patients, stethoscopes, tendon hammers,
- Watches, phones, messenger bags, masks
- WoW surface being used for aseptic procedures such as taking blood, drawing up medication etc.
Infection Prevention has also done ultraviolet maker (UV) testing to check for effective cleaning by placing UV dots on WoWs and then reviewing the WoW 24-48 hours post to check if cleaning has occurred and the dot removed by examining it under a UV torch. Asset numbers are recorded to track down the marked WoW.
How can I help stop the transmission?
Good WoW practice:
- Local monitoring and communication to staff at huddles and handovers about cleaning requirements is important. They must be cleaned at a minimum at the start of the shift or round by the doctor or nurse using the WoW and at the end. Areas and teams should develop a local process.
- Make sure no items such as sterile stock, personal clothing, medicine cups, spoons, staff drink bottles and food are placed on the WoW
- A small number of medicine cups and spoons can be placed in kidney dish for a medication round and then returned to treatment room at end of session, or they can be kept in the patient’s own medication drawer.
- Ensure Clinell wipes and hand rub are available on WoW for routine use.
- Do not eat or drink in the clinical areas.
- Ensure keyboard is cleanable and cleaned regularly as debris and soil become embedded in the keyboard grooves.
- Do not take WoWs and LoWs into isolated patient rooms or inside the bedside curtains as these curtains frequently come into direct contact by multiple hands and equipment, please use the dedicated PC in single rooms and managers ensure they are functioning.
- Do not set up for sterile procedures on the WoW, use a dressing trolley.
- Do not attach tapes to the WoW or tape paper towel to the WoW for use as a mouse pad, specific cleanable infection prevention mouse pads are available.
- WoWs are not part of the patient zone so hand hygiene must be performed between touching the patient and the WoW. If the WoW then does encounter the patient environment, then it must be cleaned.
- WoWs should be thoroughly cleaned at the end of each round, including the keyboard, mouse, and surfaces.
- Don’t place personal items on the WoW or hang it off them.
Other environmental requirements:
- Clean all shared patient equipment, stethoscopes, tendon hammers, shower chairs, hoists etc after each use on patients.
- Ensure patient rooms are not cluttered and therefore not easily cleaned.
- Patients are provided with hand wipes with their meals, encourage them to use them to reduce that oral ingestion.
- Ensure contaminated equipment, linen skips, clinical waste bins are not in close proximity to isolation trolleys, so PPE is not contaminated.
- Do not place food trays on isolation trolleys therefore contaminating PPE and surface.
- Clean isolation trolleys at beginning of each shift and don’t place sterile items on them, along with cleaning of any equipment attached to patients such as pumps, monitors, ventilators etc. which are frequently touched by multiple hands.
- Remember to always practice good hand hygiene including before and after glove use, wearing gloves does not negate the need for hand hygiene.
- Gloves should be readily available in the room and not stored outside on the isolation trolley to ensure hand hygiene is performed and gloves donned after touching the curtain or opening the door, immediately before touching the patient.
- Ensure all CPO rooms have a terminal clean with UV markers used and steam cleaning of their sinks prior to room being used again.
Communicating risk:
- Always fully complete the infectious risk screening tool on each admission and check if patients have been overseas or within another TRA declared hospital in Victoria. If yes, please refer to the CPO procedure and let Infection Prevention know.
- Always check patient infectious risk alerts on presentation and admission as there are several thousand CPO different alerts in place, read the comments in the alert and the Infection Prevention notes in EMR for guidance, never cease or resolve an infectious risk alert or cease CPO screening orders, only ID or IP undertake that. There are 2 different clearance regimes required depending on the level of contact and within set timeframes.
Bill introduced to enhance Nurse Practitioner autonomy

The Commonwealth has been undertaking work to recognise the role Nurse Practitioners and participating midwives play in the delivery of health care services, contributing to the bigger goals of the Strengthening Medicare Taskforce and the Nurse Practitioner Workforce Plan.
Nurse Practitioners are experienced registered nurses who have completed a Master’s degree. They work independently to assess and diagnose patients, request and interpret tests, prescribe medication and therapies and make referrals to other health practitioners.
Currently, nurse practitioners and endorsed midwives are prevented from autonomously providing services under Medicare and prescribing PBS medicines, without the supervision of a medical practitioner – known as a Collaborative Arrangement. An independent review found this legislated requirement creates several barriers to accessible, high-quality care for patients, particularly in rural and remote communities where it can be harder to see a doctor.
The Professional Standards for Practice, and Safety and Quality Guidelines issued by the Nursing & Midwifery Board of Australia already requires registered nurses, midwives, and nurse practitioners to engage in collaboration with other health professionals.
The Health Legislation Amendment (Removal of Requirement for a Collaborative Arrangement) Bill 2024 was introduced to Federal Parliament on 20 March 2024. If passed by Parliament, the Bill will remove the legislative need for collaborative arrangements to provide MBS services and prescribe PBS medications.
The Bill aims to:
- remove barriers to care provided by nurse practitioners and participating midwives, particularly in rural and remote areas where there:
– is a smaller healthcare workforce
– are challenges attracting and retaining GPs. - provide nurse practitioners and participating midwives more autonomy in their scope of practice
- increase use of participating midwives in First Nations settings
- support our goal of health care professionals being able to work to their full scope of practice.
Subject to passage through Parliament, the change will come into effect from 1 November 2024.
IV Paracetamol shortage

The current shortage of IV Paracetamol 1000mg/100mL vials/bag in Australia is anticipated to continue until June 2024 due to unexpected increase in demand and production delays.
Clinicians are requested to consider alternative routes of administration and to reserve the use of IV vials for situations where alternative routes are not suitable.
Western Health has limited stock available, and hence usage of stock is being monitored closely. Over the past week usage of this product has not reduced sufficiently despite various interventions, and subsequently our projected stock holdings continue to decline. Hence, we are now taking the measure of removing stock from additional Western Health imprest sites except for ICU, Theatre and Emergency Department locations.
Paracetamol suppositories have been added to all imprests currently/previously stocking IV preparations and should be used as a first-line alternative for patients unable to have oral preparations.
Please contact Pharmacy for individual requests for paracetamol IV supply in locations where it has been removed from imprest.
Our Commitment to Close the Gap

National Close the Gap Day was recently held on 21 March 2024, and recognises the national agreement to overcome inequality experienced by Aboriginal and Torres Strait Islander people and achieve life outcomes equal to non-Indigenous Australians.
Each year progress on the 19 national socio-economic targets across areas that have an impact on life outcomes for Aboriginal and Torres Strait Islander people is reported.
They range from ensuring babies are born at a healthy birthweight, supporting children to thrive, and ensuring there are appropriate pathways for education and employment.
Progress has been made, but it has been too slow and the gap is still too wide. For instance, Aboriginal and Torres Strait Islander people still have a life expectancy that is 10-11 years less than non-Indigenous Australians!
Western Health has a growing Aboriginal and Torres Strait Islander community and is committed to self-determination. As part of our efforts to close the gap we are incredibly proud of the culturally responsive care options we have designed to ensure that Aboriginal and Torres Strait Islander patients receive respectful, high-quality care with greater access and choice. These include:
- The Galinjera Maternity Program
A small team of dedicated midwives and doctors, who provide culturally-safe continuous care to Aboriginal and Torres Strait Islander families and babies. You can read more about how this service is improving outcomes for our community on our website.
- Babaneek Booboop Program
A program promoting the health and developmental outcomes of First Nations children in Melbourne’s Western Suburbs (the City of Melton and Moorabool Shire). Establishing and building on strong networks, the program supports children and their families in their engagement with child health and promotes cultural safety in health.
It won the Excellence in Aboriginal Health and Wellbeing Award at the Victorian Public Healthcare Awards in 2023. Read more.
- The Aboriginal and Torres Strait Islander Outpatient Clinic
A culturally safe, general medicine stream clinic for Aboriginal and Torres Strait Islander adults with chronic health conditions who do not require urgent care.
It is designed to provide a wrap-around service for patients with longer appointment times, a multidisciplinary focus, assistance with any barriers to attending and the individualised support and advocacy of an Aboriginal Hospital Liaison Officer (AHLO). Read more.
Wilim Berrbang Manager (Acting) Ashleigh Vandenberg and Wiradjuri woman said that everyone has a part to play in helping us achieve health equity for all Australians. “We all have a role to play in closing the gap and our actions can have a positive impact on the health and wellbeing of Aboriginal and Torres Strait Islanders and society more broadly,” Ashleigh said.
New support for Aboriginal Menal Health consumers

To improve the way we support consumers and their families seeking support with their mental health and wellbeing, Western Health has appointed our first Aboriginal Mental Health Liaison Officer in Wilim Berrbang.
Maddie DePetro (pictured right) is from the Yorta Yorta & Dja Dja Warrung clan and is passionate about ensuring Aboriginal and Torres Strait Islander patients feel heard within the healthcare system.
Referrals can be made to Maddie via the Wilim.Berrbang@wh.org.au, via phone on 0482 130 724, or on EMR select: Aboriginal health- Other- Request AMHLO support.
How can I make a difference?
You can make a difference by being educated and informed on ways you can provide culturally-safe care:
- Read more about Closing the Gap on its website. The latest report was released on 21 March.
- Read Western Health’s Cultural Safety Plan.
- Complete our cultural awareness training on WeLearn to improve your understanding of Aboriginal and Torres Strait Islander cultures, histories and successes.
- Visit the Wilim Berrbang team staff intranet page.
Benchmarking Best Care
The latest benchmark reports from the Health Roundtable that go up to September 2023 have recently been released, that show how our delivery of Best Care compares to other health services across Australasia.
Let’s look at how we perform in the area of Medication complications, which include drug related respiratory complications/depression, haemorrhagic disorder due to circulating anticoagulants, movement disorders due to psychotropic medication and serious alteration to conscious state due to psychotropic medication.
Medication Complications:
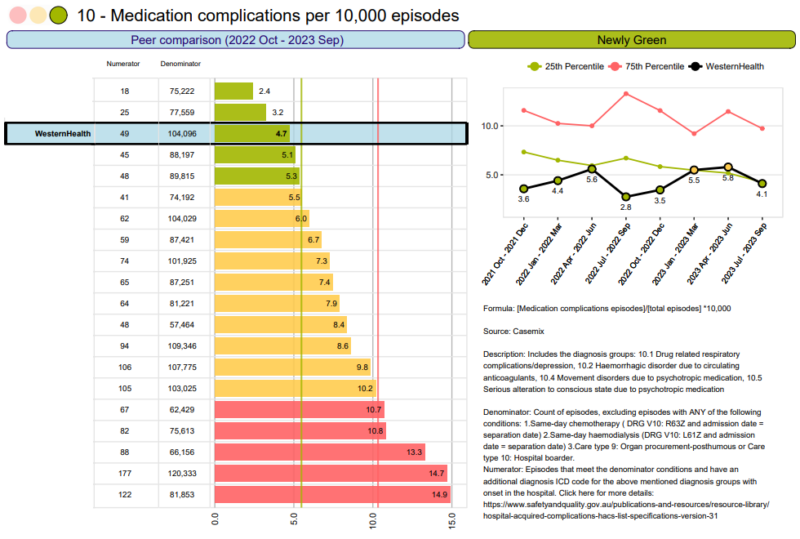
At Western Health as a whole the rates of medication complications per 10,000 episodes has been consistently green. We are amongst some of the best outcomes in Australia. This is a wonderful result.
The last quarter this has decreased again to green.
Well done to all of our Western Health teams.
Educational Opportunities

Are you ready to embark on an exciting educational journey in 2024? Please click here for details on how to apply.
Refer to the Department of Health links below to see if you qualify for the 2024 DHS Scholarships:
- Post Graduate Nursing/Midwifery scholarship information
- EN to RN DHS scholarship information
- Mental Health Post Graduate Scholarship information
- Aboriginal Nursing and Midwifery Postgraduate Scholarship Program information.
Upcoming courses being offered to Western Health nurses and midwives:
April 2024
18 – Diabetes Study Day
23 – Deteriorating Patient Study Day
23 – Stroke Study Day
24 – Preceptorship Study Day (Williamstown)
29 – Excel Introduction (9am-12pm)
29 – Excel Introduction (1pm-4pm)
30 – CVAD Workshop
30 – Surgical Advanced Study Day
May 2024
1 – Preceptorship Study Day (Bacchus Marsh)
10 – The 3’D’s – Dementia, Delirium and Depression Study Day
15 – Heart failure study day
Please visit the Education and Learning link for more courses.

