Published on 1 September 2023
Edition 71: September 2023
-
Helpful contacts
Employee Assistance Program: 1800 099 444
Nurse & Midwife Support: 1800 667 877
Nurse & Midwife Health Program: 03 9415 7551 or 1800 888 236
-
Upcoming dates
September 2023
1 Mental Health & Wellbeing Act 2022 commences
4 Endnote 20 workshop
12 VCCC Alliance Research Conference commences (Melbourne Convention & Exhibition Centre)
14 RU OK? Day
22 Research Week Abstracts due
29 Nursing & Midwifery Research Grant applications close
29 Mavis Mitchell Scholarship applications close
29 Victorian Nursing & Midwifery Trust Major Grant applications close
30 Victorian Nursing & Midwifery Trust Minor Grant applications closeCheck out Events for more details.
-
Nursing & Midwifery Executive
Adjunct Professor Shane Crowe
Executive Director of Nursing & Midwifery
Phone: 8345 1463
Email: shane.crowe@wh.org.auProfessor Bodil Rasmussen
Chair of Nursing, Deakin University/Western Health
Phone: 8395 8163
Email: bodil.rasmussen@wh.org.auDoug Mill
Director of Nursing & Midwifery
Division: Chronic & Complex Care
Phone: 0400 807 938
Email: douglas.mill@wh.orh.auHelen Sinnott
Director of Nursing & Midwifery, Sunshine
Phone: 0435 962 716
Email: helen.sinnott@wh.org.auAdjunct Associate Professor Jo Mapes
Director of Nursing & Midwifery, Footscray
Division: Perioperative and Critical Care
Phone: 0423 302 337
Email: joanne.mapes@wh.org.auKylee Ross
Acting Director of Nursing & Midwifery Informatics (CNMIO)
Phone: 0409 555 384
Email: kylee.ross@wh.org.auLena Pejcinovski
Director of Nursing, DPFC
Division: Custodial Health
Phone: 0422 818 187
Email: lena.pejcinovski@wh.org.auProfessor Linda Sweet
Chair of Midwifery, Deakin University/Western Health
Phone: 8395 1178
Email: linda.sweet@wh.org.auLisa Gatzonis
Director of Nursing & Midwifery Workforce
Phone: 9393 0127
Email: lisa.gatzonis@wh.org.auMonique Sammut
Director of Nursing & Midwifery, Sunbury
Divisions: WPHU and Clinical Support & Specialist Clinics
Phone: 0412 769 423
Email: monique.sammut@wh.org.auNicole Davies
Director of Nursing & Midwifery, Williamstown
Division: Emergency, Medicine & Access
Phone: 0435 656 190
Email: nicole.davies@wh.org.auRobyn Peel
Director of Education & Learning
Phone: 0468 608 141
Email: robyn.peel@wh.org.auRohan Vaughan
Director of Nursing & Midwifery, Melton
Division: Drug Health
Phone: 0434 365 769
Email: rohan.vaughan@wh.org.auRyan Dube
Director of Nursing
Senior Mental Health Clinical Lead
Division: Mental Health & Wellbeing
Phone: 0420 228 035
Email: ryan.dube@wh.org.auAdjunct Professor Tanya Farrell
Director of Maternity Services
Division: Women’s & Children’s
Phone: 0468 830 755
Email: tanya.farrell@wh.org.auVal Dibella
Acting Director of Nursing & Midwifery (Inspiring Innovation)
Phone: 0466 489 687
Email: val.dibella@wh.org.auWendy Giddings
Director of Nursing & Midwifery, Bacchus Marsh
Divisions: Aged, Cancer & Continuing Care and Bacchus Marsh & Melton
Phone: 0458 603 897
Email: wendy.giddings@wh.org.au
From Shane

As we enter into spring, leaving winter behind us it is great that we have been able to introduce our new COVID Sustainability Matrix and ease our COVID settings due to us being ‘green’ at the moment. This year we also had 98% of our nurses and midwives vaccinated against the seasonal flu which is an excellent result. I am grateful to you all for your continuing support in providing a safe environment for our staff, patients, volunteers and visitors.
A big welcome to our latest group of 34 new graduate nurses that commenced with us on 7 August 2023. I hope you are all starting to settle in, and I am confident that you will be getting awesome support from your colleagues.
Please join me in congratulating Dr Margie McCormick (Midwifery Educator) who recently completed her PhD!! This is a huge accomplishment, and I have been enjoying reading her thesis on Women’s Safety During Labour and Birth: A Qualitative Study. Well done Margie!
I was recently delighted to announce that Adjunct Assoc Prof Jo Mapes, Wendy Watson and Adjunct Prof Tanya Farrell have been appointed into the newly created roles of Deputy Executive Directors of Nursing & Midwifery. I am so pleased to introduce additional very senior roles into our nursing and midwifery structure at Western Health, and Jo, Wendy and Tanya will play an instrumental role in providing leadership in our professions as we continue to grow over the coming years. I was also incredibly proud that 3 internal applicants were the strongest candidates for these roles in a fiercely competitive field, a testimony to the caliber of nursing and midwifery leadership that we have in the West.
Recently Western Health initiated, coordinated and hosted a Falls Collaborative where 15 other health services from across Victoria attended a one-day session to collaborate and learn from each other. The attendees discussed falls prevention strategies in hospital, patient education, staff education and training and the world guidelines on falls prevention in hospital. My thanks to Bec Woltsche (ADONM) for initiating and implementing this forum and for her leadership in this area not only at Western Health, but across the State.
The care requirements of each of our consumers are complex and need to be tailored to their individual needs. We need to take into consideration their own goals and include them as a partner in their healthcare. It is also vital that we document this effectively and ensure that the nursing and midwifery voice is strong within the consumer’s medical record. To support this recently the EMR was updated to support a small number of preselected goals and nursing interventions in the Comprehensive Care Interdisciplinary Plan of Care (IPOC). Please make sure that you initiate a Comprehensive Care IPOC for every patient, include their specific goals and add additional interventions as required, to create an individualised plan of care. Only select interventions that are relevant to your patient, so you are not inadvertently creating ‘nuisance alerts’ in the EMR. Also please make sure that you review and update your patient’s IPOC each shift and update it as required. The IPOCs are how we document our plans, but also our nursing interventions and so are integral that this is done for every patient, every time.
As one of the final areas of focus ahead of our upcoming accreditation, over the coming months we will be focusing on ensuring consistency of practice across out departments, to ensure that we are all delivering Best Care and decreasing variance wherever possible. I encourage you all to get actively involved!
The new Mental Health& Wellbeing Act 2022 came into affect on 1 September, and a lot of information sharing and education has been occurring recently for our Mental Health & Wellbeing colleagues. Additional details and links to information and education is included below.
Finally, scholarship and grant season has commenced again and the opportunity for a number of grant and scholarship opportunities have been included below and on the Nursing & Midwifery microsite. If you are planning to study or undertake research in 2024 don’t miss out!
Shane Crowe
Executive Director, Nursing & Midwifery
Introducing our new Deputy EDONMs

It is exciting to announce the appointment of Adjunct Assoc Prof Jo Mapes, Wendy Watson and Adjunct Prof Tanya Farrell as Deputy Executive Directors of Nursing and Midwifery (DEDONM) here at Western Health.
These newly created roles are in response to the rapid growth and in preparation for the continued expansion of Western Health services over the coming years. All 3 will be well known to you all.
Jo commenced at Western Health in 2020 as the Director of Nursing and Midwifery with divisional partnership to Perioperative and Critical Care and site responsibilities of Footscray Hospital. Jo is a Fellow of the Australian College of Nursing and on the Victorian Board of the Nursing and Midwifery Board of Australia. She has extensive experience as a nursing leader and has worked in both public and private health sectors both in Australia and overseas. Her experience extends to the development and implementation of strategic change with a demonstrated capacity to lead and develop people in delivering better outcomes across systems, work units, teams and consumers.

Wendy has worked at Western Health for the last 3 as the Divisional Director for the Women’s and Children’s Services and previously for over 10 years as the Director of Nursing and Midwifery for Sunshine Hospital. Wendy has over 30 years experience in the healthcare arena within Australia, New Zealand and the United Kingdom. She is highly respected for her leadership skills, clinical expertise and commitment for high quality patient care in line with the best care framework.
Wendy’s values-based leadership style results in a positive culture within teams, strengthening team performance, driving change and delivering strategic organisational outcomes.

Tanya joined Western Health earlier this year as the Director of Maternity Services. She is a midwife and a nurse and has extensive experience, expertise and leadership within maternity at a Victorian and national level, with a proven track record of an ongoing commitment to improving the care of women and babies. Tanya was previously the Senior Maternity Adviser for Victoria at Safer Care Victoria (SCV) and has also spent time as the Acting Chief Nursing and Midwifery Officer for Victoria.
These 3 incredible internal applicants were the strongest candidates for these roles in a fiercely competitive field; a testimony to the calibre of nursing and midwifery leadership that we have at Western Health.
To ensure we have strategic alignment across the organisation, the DEDONM roles will work in partnership with the Deputy Chief Operating Officers (DCOOs) and their portfolios as follows:
- Jo Mapes will align with Jason Plant (DCOO), and lead the Directors of Nursing & Midwifery that align to Divisions in his portfolio.
- Wendy Watson will align with Paul Leyden (DCOO), and lead the Directors of Nursing & Midwifery that align to Divisions in his portfolio.
- Tanya Farrell will be our Senior Midwife and will retain her Director of Maternity Services role with a focus on Maternity Services and Women’s and Children.
Please join us in congratulating Jo, Wendy and Tanya on their appointments and wish them every success in their new roles.
Disposal of Pharmaceutical Waste

Western Health is introducing a new framework for disposing of pharmaceutical waste to comply with Victorian legislative and EPA guidelines and to minimise the environmental impact associated with pharmaceutical waste generation.
This will involve introducing pharmaceutical waste bins (termed P22) specific for medication disposal. The contents of these bins are incinerated as per EPA requirements. The bins have already been introduced in operating suites, majority of mental health wards, custodial health as well as 2 pilot wards at Footscray Hospital.
Pharmaceutical waste includes:
- Unused, unwanted or out of date medicines
- Packages, containers and equipment containing an extractable volume of a medication
- Any container or equipment that has held a Schedule 8 or 11 medicine, regardless of whether it is empty
Note: Saline, sugar, nutrient solutions and associated packaging, containers and equipment are not pharmaceutical waste.
Essentially the P22 bins are the same size and look very similar to yellow sharps bins. The distinguishing feature is an orange lid. Bins can be mounted to a wall (preferred) or placed on a trolley in the medication room.
A poster has been developed to guide medication waste disposal in clinical wards and departments. For more information, or assistance in implementing the bins, email nicole.davies@wh.org.au. or discuss with your local nurse/midwife educator or pharmacist.
Anaphylaxis Procedure update

Patients who have their own adrenaline auto-injectors must have access to it for self-administration during all healthcare encounters and clinical areas.
On admission to Western Health, all clinical staff are responsible for determining a patient’s known allergies or adverse reactions and documenting within the medical record.
All clinical staff must determine if a patient has been prescribed an adrenaline auto-injector in the community and escalate this information to the bedside nurse or midwife. If so, medical and nursing/midwifery staff should ensure “Patient has an adrenaline auto-injector in the community” alert is documented in EMR (Clinical Patient Folder for Bacchus Marsh and Melton: see Anaphylaxis PPG re: non-EMR areas). See EMR QRGs
The admitting nurse or midwife will:
- Complete “Patient’s own use of adrenaline auto-injector” Checklist on EMR, if a patient has brought in their adrenaline auto-injector.
- Provide a copy of “Use of Your Own Adrenaline Auto-Injector in Hospital” leaflet.
- Discuss with the patient/carer the most appropriate location to store their adrenaline auto-injector and Australian Society for Clinical Immunology and Allergy (ASICIA) Action Plan for Anaphylaxis (paediatric: labelled storage container, adult areas: unlocked bedside drawer, patient’s bag) and document appropriately. Anaphylaxis auto-injector bags are available if the patient prefers.
- Ensure the adrenaline auto-injector accompanies the patient when the patient temporarily leaves the ward and ensure return with the patient on discharge.
The admitting medical officer will:
- Ensure the patient has a current ASCIA Action Plan for Anaphylaxis.
- If the patient does not have a current ASCIA Action Plan for Anaphylaxis, it is the responsibility of the admitting medical officer to complete one.
- Patients who have been deemed competent to use their own adrenaline auto-injector and have access to their device should have a ‘prn’ order for the adrenaline auto-injector charted on EMR.
Please refer to the Management of Anaphylaxis Procedure for more information.
If the auto-injector is expired or not stored appropriately – a replacement pen can be ordered from pharmacy (only to replace a sighted patient’s own adrenaline auto-injector).
Encourage patients who have not brought in their own adrenaline auto-injector to have a friend/family member to bring it into hospital.
If a patient does not have their own adrenaline auto-injector and experiences anaphylaxis, the standard hospital procedure of adrenaline via ampoules applies.
Changes to Warfarin Packages

Please be aware that warfarin (Coumadin and Marevan) is now available in new packaging, similar to multiple other medication by the manufacturer Mylan/Viatris.
Both brands of warfarin, in all strengths, are now being supplied to multiple health services (and community pharmacies) in identical blue bottles. Many other medicines manufactured by Mylan/Viatris are already supplied in identical blue bottles.
As warfarin is a known high-risk medicine, the new blue packaging is a risk for selection errors and therefore medication and dose errors by pharmacy and nursing staff. Patients taking warfarin at home are also at increased risk of a selection or dosing error. These errors have the potential to result in a severe or fatal outcome.
Healthcare professionals are requested to carefully review when taking medication histories and provide patient and carers education on similar packaging where appropriate.
As an APINCH medication –it is recommended to always take extra care when prescribing, dispensing and administering warfarin.
Introduction of COVID Sustainability matrix
Western Health has continued to closely monitor the status of COVID in our facilities and across the community. This information has informed our COVID settings which have periodically escalated and de-escalated based on the level of risk.
Unfortunately, COVID will continue to remain a factor that we need to take into consideration to provide a safe environment for our staff, patients, volunteers and the public.
Based on our experience and evidence, Western Health is now moving to a COVID Sustainability matrix to inform our settings from this point forward. The matrix is outlined below and aims to provide a transparent and simplified guidance for our staff and volunteers, and includes the trigger points that we will use to inform our settings.
The matrix provides guidance on:
- masking and visitor guidance based on whether the health service is red or green:
- how settings change in wards/departments where there is a patient(s) with COVID or suspected COVID (SCOVID); and
- the definition of an outbreak ward, and control measures to be implemented if a ward/department meets this definition.
In accordance with the matrix below, Western Health’s COVID status is currently Green, therefore the relevant masking and visitor settings can be put in place in your area as outlined below. If a ward/department has patients with COVID or SCOVID or meets the definition of an outbreak ward, please continue to wear a P2/N95 respirator whilst in that environment.
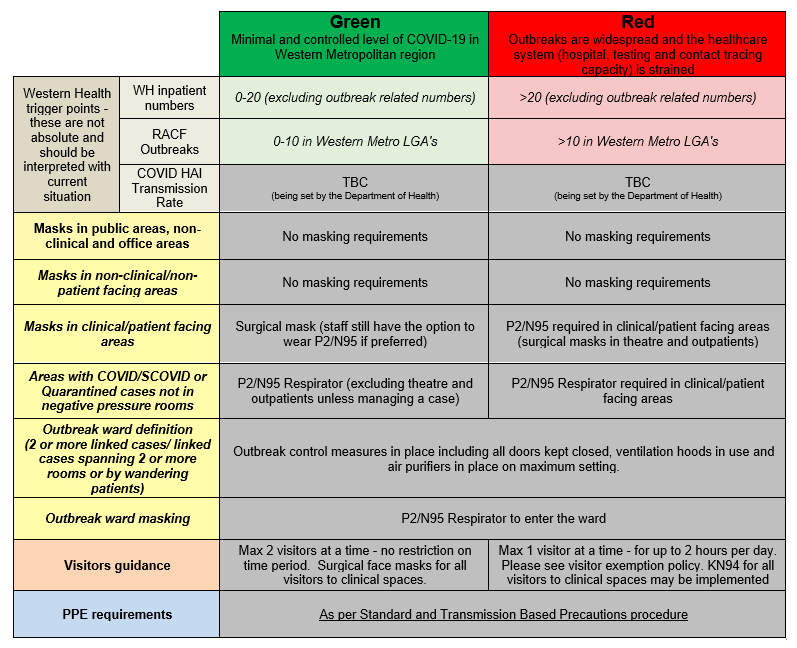
We will continue to monitor the data and will formally advise all staff and volunteers any change to our status in the future.
We continue to be committed to providing a safe environment for all of our staff, patients, volunteers and visitors and again thank you for your commitment and support.
Documenting Comprehensive Care

Recently upgrades to the Comprehensive Care IPOC will go live in the EMR. This includes a small number of preselected goals and nursing interventions. After completing the patient’s Comprehensive Care Risk Assessments, the admitting nurse must initiate a Comprehensive Care IPOC, include patient specific goals and add additional interventions as required, to create an individualised plan of care.
Every subsequent shift, each nurse must review the Comprehensive Care IPOC, and update as required. Additional interventions can be added using the ‘add to phase’ function.
Every patient requires a plan of care, hence every patient must have an individualised Comprehensive Care IPOC insitu that is reviewed and updated every shift.
Below are links to two Digital Health QRG’s if you are unfamiliar with using the Comprehensive Care IPOC:
- Comprehensive-Care-Admission-Assessment-Adult-Risk-Assessment-and-IPOC
- Clinical-Care-Nurse-Admit-and-Manage-mPages
An education package has been developed to support documenting the comprehensive care that we provide to our consumers. It outlines the essential elements of comprehensive nursing care at Western Health and where to document your information in the EMR
The intent of the comprehensive care standard is to provide person-centred care and ensure risks of harm are prevented and managed whilst the patient is in hospital.
The six elements of comprehensive care are:
- Complete a clinical assessment & identify a nursing diagnosis
- Identify the patient’s goals of care
- Complete evidence based risk screening & risk assessment
- Develop a Single comprehensive care plan
- Deliver the person centred care as planned
- Review the impact of care against the goals
Clinical Assessment:
The Nursing Assessment is where you gather the subjective and objective data related to your patient. As part of this talking with patients about their needs and preferences helps clarify what is important to them as an individual.
All patients require documentation completed on admission to identify the patient’s baseline condition. Admission documentation in the EMR includes the:
- Basic Admission Assessment including (Vital Signs and Weights), and
- Initial Patient Assessment
Goal Planning:
Talking with patients about their needs and preferences helps clarify what is important to them as an individual. Complete the “About Me” form to provide the team with information that is important to your patient. Identify who the patient/consumer wants involved in discussions, interventions and goal planning. Use the patient goals to inform the comprehensive care plan (interdisciplinary plan of care, or IPOC).
Risk Screening & Assessment:
Risk screening and assessment are a core part of comprehensive care. As well as identifying clinical issues, they also support decision making for treatment plans and risk mitigation.
The remainder of the comprehensive care risk assessment can be found in the Adult Risk Assessment which is located via the Interactive View and Fluid Balance tab. (iView)
The nursing admission note is found via the nurse view MPage
Develop a comprehensive care plan:
The Comprehensive Care IPOC details preventative actions for all risks associated with the comprehensive care standard and should be completed with every patient. It should also include patient specific goals.
Navigate to the Orders Tab in the Table of Contents. Every patient will have a Comprehensive Care IPOC in Suggested Plans. The Comprehensive Care IPOC details preventative actions for all risks associated with the comprehensive care standard and should be completed for every patient.
The individual IPOCs for components such as falls, pressure injuries, delirium, OVA only need to be initiated if that problem has already occurred. For example, the falls risk IPOC only needs to be completed if the patient has had a fall.
Despite the EMR suggesting these IPOCs, there is no need to initiate extra IPOCs unless the problem has actually occurred.
Identifying and setting goals of care in collaboration with the patient, ensures care is individualised. Having a clear, shared understanding of goals of care is increasingly important when a patient has complex healthcare issues, such as multiple comorbidities or a life-limiting illness.
Ensure you review and tick appropriate goals that reflect the patient wishes.
The interventions should be documented within the IPOC to achieve the desired outcomes e.g. falls prevention strategies.
You can add the timing of specific interventions that will be visible as a task on care compass for other members of the nursing team caring for the patient as well as referrals to allied health.
Ensure you review and tick appropriate interventions and frequency. Once you have added and reviewed the goals and interventions – ensure to initiate and sign the IPOC order.
Deliver comprehensive care:
Delivering comprehensive care should include relevant clinical disciplines working together in a multidisciplinary team to achieve the goals of care. Patients, families, carers and other support people are also essential for the delivery of comprehensive care. It is essential that all stakeholders are aware of the goals of the care plan to allow them to contribute.
The majority of day-to-day nursing & midwifery interventions are documented via Care Compass, iView and Activities & Interventions. This includes activities such as vital signs, fluid balance, management of lines and devices. Document any variations and discussions with family / carers in the nursing shift progress note.
Review comprehensive care:
Review of comprehensive care delivery involves revisiting diagnoses, clinical and personal goals of care to ensure the plan remains appropriate and effective. The care plan should be reviewed to identify changes in the patient’s condition, expectations, needs, diagnoses or prognosis.
Remember, after an IPOC has been initiated it should be reviewed each shift to ensure it is still relevant to the patient. This is done via the Document in Plan tab in the comprehensive care IPOC in the orders section of the EMR.
To track progress against existing goals, Add the target date to reach the goal. Tick if the goal has been achieved, not achieved or progressing.
The nursing shift note should also be used to document any variations in care or outcomes.
If the patient is progressing but requires additional interventions, modify additional goals or interventions by selecting the goal or intervention, right-click and select modify, update the details and sign. The nursing shift note should also be used to document any variations in care or outcomes.
To add additional goals or interventions, select “Add to Phase” then “Add outcome/Intervention”. The nursing shift note should also be used to document any variations in care or outcomes.
Patient Privacy is Paramount

A reminder that the screen on your Workstation on Wheels (WoW) contains lots of sensitive information, and we have an obligation to ensure that patient information is kept private.
Please ensure that data and information on your screen is not visible to others that should not be able to read it. This includes:
- WoWs that are not in use should not be left with information visible. Please tap-off before you leave the WoW.
- WoWs being wheeled down into public areas should not have patient information visible to others on the screen.
- It is recommended that screens that are located within corridors have a privacy screen purchased and fitted over the screen (pictured right). This allows the person in front of the screen to see the information, but anyone at an angle to have the information obsured. They are cheap and are mounted in front of the screen.
Also please remember to not send identifying patient information over unsecured communications apps like WhatsApp.
New Mental Health & Wellbeing Act now enacted

Victoria has a new Mental Health and Wellbeing Act, which was enacted from 1 September 2023. The new Act replaces the Mental Health Act 2014.
The Mental Health and Wellbeing Act supports changes underway to transform Victoria’s mental health system. The changes will deliver a new system where Victorians receive the care they need early, and in their community. The new Act is a key recommendation of the Royal Commission into Victoria’s Mental Health System.
Here you can find a list of important links, documents, and video recordings surrounding the Mental Health Act on Westerly.
The Mental Health & Wellbeing Act Training Modules are now available on WeLearn, and Mental Health & Wellbeing nurses need to complete this as soon as possible.
Key changes include:
Forms:
There are minimal changes to forms. The new forms follow the same structure as the Mental Health Act 2014 forms with updates to ensure they are compliant with the new Act. Information is still recorded in CMI.
There is one new form – MHWA-143. This is the Authority for Chemical Restraint. This form will be supported by the Chief Psychiatrist’s guidelines regarding the regulation of chemical restraint.
Statement of Rights:
Just like the 2014 Act, under the new Act, Statements of Rights must be provided to people in range of circumstances. Statements of rights are similar to the 2014 Act – but with strengthened obligations to take all reasonable steps to ensure rights are understood.
A new requirement is that a statement of rights must be provided to people admitted to bed-based designated mental health services – including people receiving services on a voluntary basis. The relevant statement of rights must be given to a person at key points during their assessment and treatment.
Nominated Support Persons:
Under the new Act, nominated person has been renamed ‘nominated support person’. The Act also clarifies the role of the nominated support person is to advocate for the views and preferences of the patient and support them to communicate and make their own decisions.
One important change is the Act removes requirements that the appointment of a nominated support person be witnessed by an authorised witness – under the Act, they can now be witnessed by any adult. The Act also makes clear that a designated mental health service must take all reasonable steps to support a nominated support person in their role.
Compulsory Treatment:
Under the new Act, compulsory assessment criteria and compulsory treatment criteria are unchanged. However, the Act introduces new rights-based decision making principles – and these principles apply to decisions made about compulsory assessment and treatment.
Decision makers must give proper consideration to these principles when exercising a power or making a decision in relation to a patient’s assessment, treatment and care. The new Act promotes voluntary treatment in preference to compulsory treatment wherever possible and requires that mental health and wellbeing services are provided with the least possible restriction of people’s rights, dignity and autonomy.
An important change is the Act reduces the maximum duration of community treatment orders from 12 months to 6 months. The provisions regarding the Mental Health Tribunal are comparable to those of the Mental Health Act 2014 with some minor changes.
Advance Statement of Preferences:
Advance statements’ under the 2014 Act have been renamed ‘advance statement of preferences’ in the new Act. The new Act clarifies that statements can include preferences about any aspects of care and support, not just treatment preferences.
One important change is the Act removes requirements that advance statements be witnessed by an authorised witness – under the new Act they can now be witnessed by any adult. A designated mental health service must also ensure all reasonable efforts are made to give effect to the statement.
An authorised psychiatrist must provide written reasons within 10 business days whenever a treatment decision is made that does not accord with treatment preferences, expressed in an advance statement of preferences.
Thank you Bodil!

Professor Bodil Rasmussen has informed me for her intention to step down as Western Health’s Chair of Nursing at the end of 2023.
Bodil has been Western Health’s inaugural Chair of Nursing, and over the past 7 years Bodil has made a remarkable and long-term positive impact on nursing at Western Health. Her leadership, passion and approach has supported our nurses to significantly grow their research capability and critical thinking.
Bodil’s achievements over her time at Western Health are truly amazing, with our nurses now publishing on a monthly basis, regularly presenting at conferences, compiling posters and undertaking projects in a robust way. Bodil has connected our nurses with academic colleagues from across the world, making for excellent opportunities to learn and collaborate. None of this would have been possible without Bodil, and I am sincerely and forever grateful.
Bodil has also been a strong and respected member of the Nursing and Midwifery Executive team, and her expertise, insights, advice and counsel has always added value and resulted in better, more well-informed decisions. It has been a privilege to work closely with Bodil, and she will leave an enduring legacy.
Bodil will finish in her role on 31 December, and she has agreed to support the transition of her successor. The process to appoint our next Chair in Nursing will take place over the coming months.
Nursing & Midwifery Research Grants now open

We are delighted to announce a call for abstracts and grant applications in preparation for the Research Week 2023 (15-20 October) with the Nursing and Midwifery session being facilitated Thursday 19 October 2-4pm.
Research Grants:
The Executive Director of Nursing and Midwifery is seeking applications from Western Health staff for grant funding to undertake dedicated nursing and/or midwifery-led research.
There are three research grants to be awarded this year:
- The Western Health Nursing Research Grant, for nursing-related projects (up to $15,000)
- The Western Health Midwifery Research Grant, for midwifery-related projects (up to $15,000)
- The Denise Paterson Research Grant of $10,000 is open to a nurse or midwife.
Details of the how to apply for one of the grants is on the Research Week and Research Grants page.
Abstracts:
We are also seeking applications from Western Health Nursing and Midwifery staff to present research and or clinical audits that foster Best Care at Western Health. This year we have two types of presentations available, oral and poster presentations. As an incentive, this year we are delighted to announce there will be a $250 prize for the best oral presentation and $250 for the best poster presentation.
Oral presentation
There will be four to six 10 to 15-minute oral presentations on the day. The best presentation prize will be decided by visiting academics and announced on the day.
E-Poster
There will be an unlimited number of e-poster presentations. Posters will be required as a single PowerPoint slide made into a PDF file and will be made available on the Nursing and Midwifery microsite 2 weeks prior to Research and Best Care Week. E-Posters can be a new presentation or something you have created during the pandemic and have not yet been able to display at Western Health. Western Health staff will be invited to vote for the best e-poster via an anonymous survey. The prize will be awarded to the highest scoring poster and announced on the day.
These are exciting opportunities for nurses and midwives to be innovative, lead research, and contribute to an improvement in practice and better patient outcomes.
The abstracts is due 22 September and closing day for grant applications are 29 September 2023.
If you want to discuss your ideas or would like assistance to write the abstract and grant application, please get in touch with the Western Health-Deakin University Partnership team.
Chance to participate in our RUSON/M study

You are invited to participate in our study ‘Exploring the experiences and career trajectory of Registered Undergraduate Students of Nursing and Midwifery’.
The aim of this project is to investigate the perceptions and experiences of Registered Undergraduate Students of Nursing (RUSON) and Midwives (RUSOM) working in Victorian health services. The findings will be used to inform strategies to support Registered Undergraduate Students of Nursing and Midwives in the workplace and their transition to professional practice.
This study is being conducted by the Deakin University Centre for Quality and Patient Safety Research – which has collaborative partnerships with Alfred Health, Barwon Health, Eastern Health, Epworth Health, Monash Health, and Western Health. We would like to invite you to participate in an online survey, which will take about 5-10 minutes to complete, about your perspectives and experiences of being a RUSON or RUSOM or having RUSONs or RUSOMs working in your health service.
You can read the Plain Language Statement, which explains more about the study and what participation involves. After reading the Plain Language Statement, if you would like to participate, please click on the link https://tinyurl.com/RUSON-RUSOM to start the survey. Participation in this research is voluntary. If you do not wish to take part, you do not have to. Non-participation will not affect your employment, or your relationship with the researchers and Deakin University.
If you have any questions about the study, please contact the principal investigator, Professor Linda Sweet, on (03) 9244 5836 or email l.sweet@deakin.edu.au.
Thank you for your interest in this study.
A conversation could change a life

Do you know how the people in your world are really going? Thursday September 14 is RU OK Day, and a good reminder to keep an eye our for the wellbeing of yourself and others.
Got a feeling that someone you know or care about it isn’t behaving as they normally would? Perhaps they seem out of sorts? More agitated or withdrawn? Or they’re just not themselves. Trust that gut instinct and act on it. Learn more about the signs and when it’s time to ask R U OK? here.
Life’s ups and downs happen to all of us. So chances are someone you know might be struggling. Your genuine support can make a difference whatever they are facing, big or small.
So, don’t wait until someone’s visibly distressed or in crisis. Make a moment meaningful and ask them how they’re really going.
By starting a conversation and commenting on the changes you’ve noticed, you could help that family member, friend or workmate open up. If they say they are not ok, you can follow the recommended conversation steps to show them they’re supported and help them find strategies to better manage the load:
Be ready
- Are you in a good headspace?
- Are you willing to genuinely listen?
- Have you set aside the time you might need?
Be prepared
- Remember that you won’t have all the answers (and that’s OK).
- It can be difficult for people to talk about personal struggles and they might be emotional, embarrassed or upset.
Pick your moment
- Have you chosen somewhere relatively private where you’ll both be comfortable to chat?
- When is a good time for them to have a meaningful chat?
- If they don’t have time when you first approach them, arrange another time for the conversation.
- It might be more comfortable for the person to be side-by-side with you (e.g. walking together or sitting in the car) rather than face-to-face.
Once they’ve opened up, encourage them to access support or to do something that might lighten the load. You don’t have to have the answers or be able to offer professional health advice, but you can help them consider the next steps and actions they can take to manage their situation.
Some good options might include talking to family, a trusted friend, their doctor or another appropriate health professional. You can also suggest they think about what’s worked for them or helped in the past when they’ve felt this way or faced similar challenges.
Things that help them relax or bring them joy might include going for a walk, seeing a movie, watching or playing some sport etc.
Don’t forget to check back in on them.
Are they really OK? Ask them today. Your conversation could change a life.
If they are ok, that person will know you’re someone who cares enough to ask.
Australian College of Nursing Scholarships

ACN is proud to administer several government-funded scholarships on behalf of the Australian Government and the Department of Health and Aged Care to enable nurses and other healthcare professionals to pursue and progress their careers.
Applications for the Aged Care Nursing and Allied Health Scholarships and Puggy Hunter Memorial Scholarship Scheme are now open.
The Aged Care Scholarships are aimed at supporting both personal care workers and nurses to complete relevant qualifications. Meanwhile, the Allied Health Scholarships are geared towards assisting allied health professionals in their journey to acquire dementia-related qualifications.
The Puggy Hunter Memorial Scholarship Scheme provides financial assistance to Aboriginal and/or Torres Strait Islander students who are undertaking an undergraduate course in an eligible health-related discipline.
Head to the ACN scholarships page to learn more and apply.
ABC showcases our midwives

The ABC recently did a story on our midwives within Joan Kirner Women’s & Children’s, as an inside look into one of Melbourne’s busiest maternity wards. Our midwives work day and night to deliver thousands of babies every year. The story covered the issues being faced across the country regarding midwifery workforce shortages.
The pandemic has also exacerbated many pressures that were starting to emerge before 2020, says Tanya Farrell, the Director of Maternity Services at Western Health. “Like all services, we have had challenges in attracting midwives because the pool of midwives available to us lessened,” she says.
After a challenging few years, workforce pressures have eased at Joan Kirner with the return of healthcare workers from overseas, following the lifting of COVID-19 restrictions.
The hospital has also significantly increased the number of graduate midwives it accepts every year – from 20 to 70 – and introduced clinical educators to ensure its junior midwives are well supported.
Offering different models of care, including midwifery group practice and a home birth program, has also helped to attract and retain staff, maternity services director Tanya Farrell says.
“Our ultimate aim is to make sure that midwives can contribute to the work that they love for as many hours as they can,” she says.
“The challenge, however, is I still have to run a 24/7 service. Women need midwives to be here when the sun goes down.”
Check out the full ABC story here or watch the TV report which was aired on 6 August 2023.
Preterm and early term birth prevention education evening

Safer Care Victoria is hosting a free educational evening on Preterm and early term birth prevention.
The evening includes a complimentary dinner and presentations from key national and Victorian preterm birth prevention obstetricians and fetal medicine specialists. They’ll discuss optimal timing of birth and cervical length measurement and management. This is a rare opportunity to gain valuable insights into the Every Week Counts – National Preterm Birth Prevention Collaborative and its strategies to prevent preterm and early term births.
Select your preferred location:
Date: Monday 2 October 2023
Time: 6 pm – 9 pm (Please arrive by 5.30 pm tor register)
Location: Sofitel Melbourne – Grand Ballroom, 25 Collins Street, Melbourne 3000
Register: Visit website to register
OR
Date: Tuesday 3 October 2023
Time: 6pm – 9 pm (Please arrive by 5.30 pm tor register)
Location: Novotel Geelong – 10-14 Eastern Beach Road, Geelong Victoria 3220
Register: Visit website to register
For more information, please contact:
Victorian Preterm Birth Prevention Education Program
Improvement Branch | Safer Care Victoria
E: pretermbirthprevention@safercare.vic.gov.au
T: 03 9821 6003
Compassion is an antidote to burnout

On Thursday 24 August 2023 Western Health hosted Professor Jane Clemensen from the University of Southern Denmark, who gave an enlightening presentation on Compassion as antidote to burnout: compassion fatigue as a global challenge for healthcare.
Jane (pictured in the center right, with Shane Crowe and Assoc Prof Deb Kerr) is a pioneer, both in the field of Health Technology and in Participatory Design in Health Sciences. She is the Head of the Centre for Compassion in the Healthcare Sector, a well-known speaker at national and international conferences, and is regularly in the media for her work. In 2017, she won the award for Researcher of the Year at the Faculty of Health Sciences at the University of Southern Denmark.
For the last 20 years, Jane has collaborated with Professor Anthony Smith at the Centre of Online Health in Brisbane and in June 2023, was appointed as an adjunct professor at the University of Queensland Centre for Health Services Research.
Jane spoke to the audience about the power of compassion in overcoming suffering, and how patients can tell who truly cares about them by the compassion that is shown whilst care is delivered.
Jane spoke about how it doesn’t take any extra time to show compassion as we care for patients – sometimes it’s a smile, or a touch, or how we word things to show we care. The positive impact of that compassion on our patients makes a huge difference.
Of course, being compassionate to each other is also hugely important and makes a huge impact on job satisfaction.
Compassion is our first Western Health value, and Jane encouraged use all to strengthen out ‘compassion muscles’ through giving them a workout through practice – the more we do it, the easier it gets – and it makes us feel good too and can help prevent burnout.
VCCC Beyond the Breakthroughs Conference

As an active member of the VCCC Alliance, Western Health is part of Australia’s leading comprehensive cancer partnership. The forthcoming Research Conference on 12-13 September 2023 is a fantastic opportunity for the broader cancer research community to come together – all disciplines, specialities and tumour streams are covered.
The program includes some exceptional international and national speakers, discussions on some hot topics, plus a range of professional workshops and a public Cancer Communities Forum. Based on the theme of Beyond the Breakthroughs, the conference emphasises implementation, translation, and equity; highlighting the integrated nature of a comprehensive cancer approach.
It would be great to see strong representation from Western Health at the event, to make important new connections and come away feeling inspired and informed.
Register for one day, both days, preconference workshops, community forum and/or the conference dinner.
New Mental Health & Wellbeing building nearing completion

For those of you that work at Sunshine Hospital, it has been impossible to not notice the large new Mental Health & Wellbeing facility being built adjacent to SAAPU on the site.
On Thursday 3 August 2023 the construction phase was officially ceased, and the building was handed over to Western Health. Since that time landscaping has been completed, and the furniture, fittings and equipment has gradually been moved into the building.
The building is huge, comprising 52 beds in total – made up of two extremely spacious 26-bed wards. One ward is on the ground floor, and the other is on the first level. The second level comprises offices. Each of the wards have a number of secure courtyards and outdoor spaces, including a basketball court! There are also numerous lounges, activity and relaxation spaces for the consumers to use. Each consumer will have significantly more space than they do in the existing facilities.
In a number of locations local artists have painted beautiful murals onto walls within the facility (an example pictured right with Executive Director of Strategy & Partnerships Susan Wardle), as well as in the new link corridor between the Emergency Department/Operating Theatres and the new facility.
The Mental Health & Wellbeing team are busy preparing for the upcoming transition into the building, where SAAPU will transition into the facility later this year.
Getting ready for Accreditation

Then any time between 1 July 2023 and 31 December 2023, a short-notice assessments will be undertaken for all of Western Health with 24 hours notice. Our mental health services will be included in our survey. We will be notified on a Thursday that a week long survey will commence on the next Monday.
We will have a team of approximately 13 accreditation surveyors visiting all of our campuses and over a week. The surveyors will spend up to 75% of survey time in clinical wards and departments.
Dame Phyllis Frost Centre will align with the new Primary & Community Health Accreditation Scheme that has a scheduled, separate accreditation survey.
What can I do to be ready?
To get ready, as you are working in your department try to look through a surveyor’s eyes:
- remove outdates or unnecessary posters and information on walls
- get rid of excessive clutter
- ensure WOW drawers are locked and are clean inside
- ensure linen trolleys are always covered
- ensure that equipment that has been cleaned has a green tag on it
- ensure cleaning schedules are visible
- ensure daily checks eg resuscitation trolley are recorded
- ensure you are able to confidently navigate the EMR in front of a surveyor
- make sure that medication and sterile stock rooms are always cleaned
- maintain a focus on the privacy of patient information
Over the coming months we will be focusing on ensuring consistency of practice across out departments, to ensure that we are all delivering Best Care everywhere, every time.
Victorian Nursing and Midwifery Trust 2024 grants applications now open

The Victorian Nursing and Midwifery Trust 2024 grants and fellowships are now open.
Major Grants:
Major Grants available for the 2024 round include:
VNMT Major Grant Up to $100,000: The purpose of this grant is to provide funding to health services to undertake dedicated nursing and/or midwifery research and education. Health Services are invited to apply for up to $100,000 for disbursement in 2024. Applications close September 29th, 2023
VNMT PhD Completion Support Grant Up to $40,000: Up to $40K to support a nurse or midwife currently undertaking a PhD in an area of nursing/midwife practice. Applicants must have completed the ethics approval process and confirmation of candidature or equivalent process. Funding is for 2024. Applications close September 29th, 2023
VNMT PhD Scholarship $40,000 each year, for 3 years: Up to $120K over 3 years of full-time study (with a maximum of $40K pa). Applications close September 29th, 2023
Minor Grants:
Minor Grants for the 2024 round include:
VNMT Post Graduate Qualification (Masters/Grad Dip/Grad Cert) Up to $10,000: Up to $10K for nurses and midwives in the final year of study in an approved full fee-paying postgraduate course in the speciality areas. Focus area for 2024 is anaesthetics, perioperative or intraoperative nursing. Applications close September 30th, 2023
VNMT Diploma/Certificate IV/ Short Courses Up to $5,000: Up to $5K to enable nurses and midwives with a minimum of 2 years in the workforce post degree to undertake post graduate short courses or activities that will enhance their practice. Applications close September 30th, 2023.
VNMT Enrolled Nurse Up to $5,000: Up to $5K for enrolled nurses to undertake professional development activities that enhance their practice as an EN. Applications close September 30th, 2023
William Cooper $5,000: The purpose of this grant is to enable nurses, involved in caring for patients with cancer in Victoria. Applications close September 30th, 2023
Rosemary Kelley Foundation $10,000 – $20,000: The purpose of this grant is to enable nurses who are directly or indirectly involved with the care of patients with haematological malignancies and other forms of cancer. Applications close September 30th, 2023
Applications are submitted electronically via the Victorian Nurses and Midwives Trust website.
Any questions regarding the grants and fellowships may be directed to info@vnmt.org or 1800 559 136.
Milestone for New Footscray Hospital

Cranes have started coming down at the new Footscray Hospital site, which for more than a year was home to the most cranes in the Southern Hemisphere. The new facility has now reached its maximum height, marking the completion of structural works on the main hospital tower. With the first three buildings in the precinct ‘topped out’ earlier this year, the hospital’s main clinical buildings are the latest to reach the milestone, including the 10-storey inpatient unit tower.
This tower is located along Geelong Road and will include the new emergency department, more than 500 beds and feature a garden at the end of each wing where patients can enjoy views across Melbourne. The sub-acute building on Ballarat Road will include the ambulatory care precinct and clinics like allied health, clinical trials and a wellness hub with a rooftop café. The design of these buildings has been carefully considered to create a welcoming and healing atmosphere for patients, families and staff.
The new hospital will be home to 50 mental health beds, 16 alcohol and or other drugs (AOD) beds, and a mental health and AOD hub – ensuring people who need urgent care get tailored, specialised and fast-tracked treatment.
With more than 150,000 tonnes of concrete poured onsite to complete the structure of the new hospital, works will now focus on the façade and internal fit-out of the hospital as it moves towards completion in 2025.
Mechanical Restraints - EMR

Following an extensive review process and engagement with relevant stakeholders, on Monday 25th September 2023 the initiation of mechanical restraints and completion of a restraint medical review, for patients who are not under the Mental Health Act, will go live in the EMR.
To prepare for this, the following educational supports are now available:
- In-services are being delivered by the Clinical Education Team
- A short WeLearn package has been developed by the Digital Health Training Team – simply search for Mechanical Restraints in WeLearn
- A workflow Quick Reference Guide is available on the Digital Health Information site Documentation – Restraint Initiation and Medical Review
From Monday 25th September, Medical – Duty of Care Restraints (Type 1 & 2) will change as below;
- The new Restraints Powerforms will be located in the AdHoc folder and will be accessed via the Basic Care folder in PowerChart or the Emergency Documents folder in FirstNet.
- The Restraint Authorisation and Alternative Restraint Strategies will be documented in the Restraint Authorisation of a Person Restrained NOT Under the MHA PowerForm.
- The Restraint Medical Review will be documented in the Restraint Medical Review of a Person Restrained NOT under the MHA PowerForm.
- Once completed, you will be able to view both documents in the Documentation tab in the Table of Contents
Staff who utilise Mechanical Restraints should complete the WeLearn lesson prior to these changes coming into place to ensure they are familiar with these workflows.
For those patients who are restrained under the Mental Health Act the following workflows will continue to be completed on paper:
- Restrictive Intervention Authorisation
- Restrictive Intervention Medical Review
- Approval For Urgent Physical Restraint
Nursing Observation documentation will be in Interactive View in the EMR.
The Digital Health Team wish to thank all those involved in the consultation, review, engagement and education of this important piece of work.
If you have any queries please contact Barbara Lennon, Acting Director, Nursing & Midwifery Informatics – Barbara.Lennon@wh.org.au
Benchmarking Best Care
The latest benchmark reports from the Health Roundtable that go up to March 2023 have recently been released, that show how our delivery of Best Care compares to other health services across Australasia.
Let’s look at how we perform in the area of Medication complications, which include drug related respiratory complications/depression, haemorrhagic disorder due to circulating anticoagulants, movement disorders due to psychotropic medication and serious alteration to conscious state due to psychotropic medication.
Medication Complications:
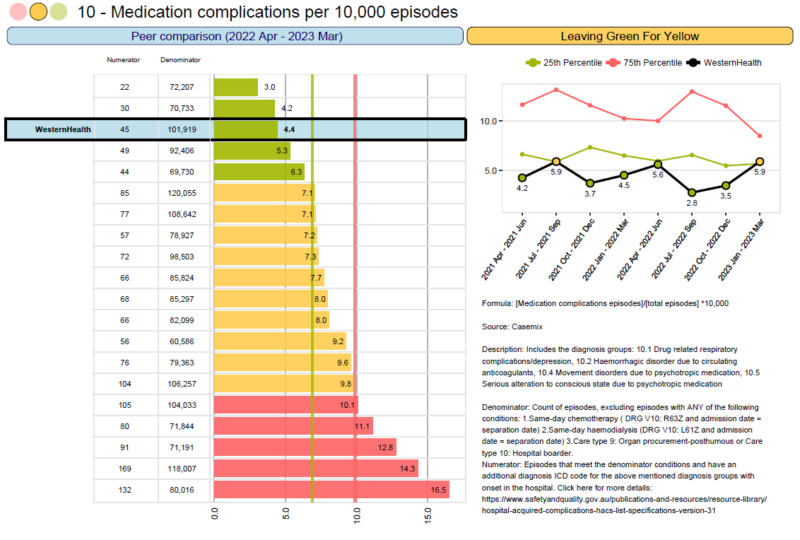
At Western Health as a whole the rates of medication complications per 10,000 episodes has been consistently green. We are amongst some of the best outcomes in Australia. This is a wonderful result.
Well done to all of our Western Health teams.
Educational Opportunities

Resuscitation Mandatory Competencies:
Sessions have recommenced. In the first instance, you can arrange an assessment with your local instructor or educator. Resus educators are contacting managers to arrange local sessions for individual teams. Dedicated sessions for Bank and Pool Staff along with sessions for Nursing and Medical staff are available on WeLearn. You can locate sessions by clicking on this link: Course: Basic Life Support (BLS) (wh.org.au)
Adult Deteriorating Patient (non-obstetric):
Learning how to recognise and escalate patient deterioration is now here at Western Health. The Education and Learning Department have developed a new and improved WeLearn course, designed to guide and support early recognition and escalation for a patient deteriorating within Western Health.
Fisher and Paykel Respiratory Support training:
RSVP to: education.australia@fphcare.com.au
- Adult & Paediatric Respiratory Support: Wednesday 4 October 2023 – WCHRE Lecture Theatre: 9.00am to 1.00pm
Education and Learning upcoming events:
- 05/09/2023: Cognitive Study Day
- 21/09/2023: Infection Prevention Study Day
- 27/10/2023: Mental Health First Aid
- 03/11/2023: Mental Health First Aid
More courses click here: Courses and Inservices (westernhealth.org.au)
Course Enrolment/Inquiries:
- WeLearn Helpdesk Email: welearn@wh.org.au
- WeLearn Enrolment link: welearn@wh.org.au
Emerging Evidence
The Western Health Library Service is a great source for locating the latest nursing and midwifery related evidence-based practice and research.
Latest articles of interest:
- xxx
New Nursing/Midwifery eBooks
- xxx
View all recently added print and eBook catalogue titles
Accessing the Library at Work:
All eligible staff can access electronic library resources from any networked PC or device connected to Wi-Fi network without the need to login.
Accessing the Library Remotely (offsite access):
- When accessing electronic resources through the library website from offsite you will automatically be asked to enter your library membership number and surname.
- Library Membership is free and can be completed online. Please email the library if you experience issues when registering (e.g. error messages).
For more information please contact the Western Health library team.

