Published on 1 May 2023
Edition 67: May 2023
-
Helpful contacts
Employee Assistance Program: 1800 099 444
Nurse & Midwife Support: 1800 667 877
Nurse & Midwife Health Program: 03 9415 7551 or 1800 888 236
-
Upcoming dates
May 2023
1 National Heart Health Awareness Week commences
5 International Day of the Midwife
11 Advancing Frontline Leadership program (Group 2)
12 Western Health’s International Nurses and Midwives Week celebration (2pm)
12 International Nurses Day
15 Aboriginal and/or Torres Strait Islander Community of Practice
16 Transforming Leadership Capabilities program (Group 2)
17 Qualitative Research workshop
23 Transforming Leadership Capabilities program (Group 2)
25 Advancing Frontline Leadership program (Group 2)
27 Palliative Care Week commences
31 Nursing and midwifery registration due (to avoid late fee)Check out Events for more details.
-
Nursing & Midwifery Executive
Adjunct Professor Shane Crowe
Executive Director of Nursing & Midwifery
Phone: 8345 1463
Email: shane.crowe@wh.org.auProfessor Bodil Rasmussen
Chair of Nursing, Deakin University/Western Health
Phone: 8395 8163
Email: bodil.rasmussen@wh.org.auDoug Mill
Director of Nursing & Midwifery
Division: Chronic & Complex Care
Phone: 0400 807 938
Email: douglas.mill@wh.orh.auHelen Sinnott
Director of Nursing & Midwifery, Sunshine
Phone: 0435 962 716
Email: helen.sinnott@wh.org.auJo Mapes
Director of Nursing & Midwifery, Footscray
Division: Perioperative and Critical Care
Phone: 0423 302 337
Email: joanne.mapes@wh.org.auKate Renzenbrink
Director of Nursing & Midwifery Informatics (CNMIO)
Phone: 0425 772 324
Email: kate.renzenbrink@wh.org.auProfessor Linda Sweet
Chair of Midwifery, Deakin University/Western Health
Phone: 8395 1178
Email: linda.sweet@wh.org.auLisa Gatzonis
Director of Nursing & Midwifery Workforce
Phone: 9393 0127
Email: lisa.gatzonis@wh.org.auMonique Sammut
Director of Nursing & Midwifery, Sunbury
Divisions: WPHU and Clinical Support & Specialist Clinics
Phone: 0412 769 423
Email: monique.sammut@wh.org.auNicole Davies
Director of Nursing & Midwifery, Williamstown
Division: Emergency, Medicine & Access
Phone: 0435 656 190
Email: nicole.davies@wh.org.auRohan Vaughan
Director of Nursing & Midwifery, Melton
Division: Drug Health
Phone: 0434 365 769
Email: rohan.vaughan@wh.org.auRyan Dube
Director of Nursing
Senior Mental Health Clinical Lead
Division: Mental Health & Wellbeing
Phone: 0420 228 035
Email: ryan.dube@wh.org.auAdjunct Professor Tanya Farrell
Director of Maternity Services
Division: Women’s & Children’s
Phone: 0468 830 755
Email: tanya.farrell@wh.org.auVal Dibella
Acting Director of Nursing & Midwifery (Inspiring Innovation)
Phone: 0466 489 687
Email: val.dibella@wh.org.auWendy Giddings
Director of Nursing & Midwifery, Bacchus Marsh
Divisions: Aged, Cancer & Continuing Care and Bacchus Marsh & Melton
Phone: 0458 603 897
Email: wendy.giddings@wh.org.au
From Shane

During May we celebrate both the International Day of the Midwife on 5 May and International Nurses Day on 12 May, which are opportunities to recogise the impact that the professions have on the community. We will be holding an event to honour both professions on 12 May at 2:00pm. The event will include our own Tanya Farrell giving the keynote address and you will be entertained and get a laugh from award-winning nurse-comedian Georgie Carroll!
There will also be some surprises throughout the week.
I am so proud of the awesome efforts of our nurses and midwives who continue to provide Best Care to our community. Every day you share your skills, knowledge and expertise with care and kindness to those in our community that need it most. All of you make a very real and tangible difference to those in our care and their families, and you will be remembered by them all for a long time after they leave us.
We are team-based professions. Teamwork, camaraderie, kindness and care are core to our professions, are these professional values make us all collectively stronger. Working in healthcare is challenging, but the care and support that you provide each other is hugely important.

This month during International Nurses & Midwives Week we will be launching our new Professional Practice Framework. The Framework has been developed after extensive consultation with our nurses and midwives, and is structured around the five domains of practice:
- leadership,
- research,
- evidence-based practice,
- education, and
- clinical expertise.
These domains are surrounded by the Best Care domains and are informed by our Values – which all together enable us to deliver Best Care to the community.
The Framework is for you, and all about you and your successful and enriching career at Western Health. It includes an achievement model of skill acquisition, to support career planning and progression and outlines the support and opportunities available to assist both the development of individuals and teams. It also offers career pathway guidance for those wishing to advance and provides consistent professional advice, assists workforce planning, and will be an invaluable resource for our staff and the wider Western Health team.
The Framework will inform important enabling documents, including our position descriptions and performance and development plans. encourage you to review the document once it has been formally released.
A huge thank you to all of our nurses and midwives to the significant positive impact that you all make to our community each and every day. I hope you all find some time in your busy days this week to celebrate our professions.
Shane Crowe
Executive Director, Nursing & Midwifery
Celebrating our nurses and midwives

In May each year we formally recognise the impact that our nurses and midwives have on the community, to coincide with the International Day of the Midwife and International Nurses Day.
The International Council of Nurses theme for International Nurses Day 2023 is Our Nurses. Our Future. In order to address the global health challenges and improve global health for all, we need to learn from the lessons of the pandemic and translate these into actions for the future that ensure nurses are protected, respected and valued.
This year’s theme for the International Day of the Midwife is Together again: from evidence to reality is a nod to the upcoming 33rd ICM Triennial Congress, where the global midwife community will come together for the first time in more than five years. It is also honours the efforts of midwives to action critical evidence towards meaningful change for the profession and the women and families our midwives care for.
Western Health’s celebrations:
This year we will be honouring both professions with an event on Friday 12 May 2023 at 2:00pm – 3:00pm in the Auditorium at Sunshine Hospital (reserve a seat – capacity 200 attendees) and virtually on Zoom (Meeting ID: 964 6016 9452 Passcode: 120859):
- Hear from our Executive Director of Nursing & Midwifery Adjunct Professor Shane Crowe, who will also be launching Western Health’s new Nursing & Midwifery Professional Practice Framework.
- Be inspired by the keynote address from Adjunct Professor Tanya Farrell, our new Director of Maternity Services. Tanya has previously been Victoria’s Senior Maternity Advisor and the Executive Director of Midwifery & Nursing at the Royal Women’s.
- Be entertained by award-winning nurse-comedian Georgie Carroll. Her bluntness and charm coupled with razor-sharp wit will give you a great laugh. Georgie had written 7 solo nationally sold-out stand up shows, and is a familiar face on Australian TV.
Enjoy delicious catering after the event in the Atrium.
There will also be some surprises for our nurses and midwives throughout the week.
Getting ready for Accreditation
![]()
The Standards of the Fortnight continue through May, with 3 Standards being covered this month:
- 1 May – 5 May – will be the final week of Standard 5 Comprehensive Care being the focus.
- 8 May – 19 May – Standard 6 Communicating for Safety will be the Standard of the Fortnight
- 22 May – 26 May – will be a week dedicated to Standard 1 Clinical Governance
For each Standard you are encouraged to get involved in the range of activities planned that are aimed to support staff to build their confidence and knowledge of the requirements of each of the Standards, so that you can show-off your achievements when the surveyors are here.
Activities include:

- Best Care Coordinator and Fab Five Walkarounds
- Q&As for front line staff
- Best Care Carnival – short, fun activities/games, online pop quizzes for each Standard with prizes
- Spotlight on the Live Best Care site on Standard per fortnight
- Behind the scenes videos of each Standard – how each relates to a range of teams and staff and to introduce Fab 5 teams
All clinical areas/departments will be visited by Best Care Coordinators within the space of the fortnight for each Standard.
To get up-to-date with accreditation readiness for each Standard, there are also bulletins and Accreditation Readiness Fact Sheets on each Standard.
Fab 5 Team Members for that Standard will also be visible around the campuses during that fortnight.

What else can I do to be ready?
In addition to joining in the Standard of the Fortnight events, you can also:
- Ensure your area and department is clean, safe and organised.
- We all love to keep pieces of equipment in store rooms just in case we might need them again one day even though we haven’t used them for the last 3 years. If you haven’t used it for the past three years, it’s highly unlikely you are ever going to use it again. Make sure you throw out old pieces of equipment and get them taken off the asset register if they are of that value. If things are broken and can’t be repaired, throw them out and get them replaced.
- Think about things we give our patients – patient information leaflets, patient education materials, to sure they are updated and reflect best practice is really important.
- Make sure you have all undertaken your mandatory education and training.
- Make sure you are working with your manager to ensure you’ve had an annual performance and development review.
The Live Best Care site is a great resource for all of our staff. There are new resources going on that almost daily. There are checklists, Q&As, and information on all of the standards and requirements, aimed at different roles. You are encouraged to check the site regularly and just make sure you’ve done everything to feel informed.
Mock accreditation:
Sometime during May and June we will be having a short notice mock accreditation. We have a very experienced surveyor coming in who is really friendly but thorough. They will come in and go around and undertake a mock accreditation with our staff. That will allow us to identify anything we might need to spend time and effort on in the last couple of weeks and months ahead of whenever our real short notice assessment is undertaken to make sure we are absolutely ready.
We’ve got this!
Registration Renewal time

The annual renewal of nurses and midwives registration lets the public and your colleagues know that you’re still safe to practise.
To avoid a late fee renew online before 31 May 2023. All nurses and midwives needing to have renewed their registration prior to 30 June 2023 to allow them to continue to practise.
Western Health does not employ anyone into any nursing or midwifery position without an active registration for any period.
Payment:
To ensure quick and effective renewal, nurses and midwives and encouraged to renew online.
Renewal fees can be paid by credit/debit card. If you do not have a credit/debit card you can purchase a pre-paid debit card from various retail outlets for a nominal fee.
Non-practicing registration:
Every year Western Health has a large number of nurses and midwives go on some extended leave. Often this is for something like maternity leave or long service leave, where they fully intend to return to work following their leave.
Occasionally some of our nurses or midwives have fallen into the trap of applying for non-practicing registration during their leave, which has impaired their ease of returning to work.
The Nursing and Midwifery Board of Australia (NMBA) regulates the practice of nursing and midwifery in Australia, and one of its key roles is to protect the public. The NMBA does this by developing registration standards, professional codes, guidelines and standards for practice which together establish the requirements for the professional and safe practice of nurses and midwives in Australia.
The types of registration available to nurses and midwives who apply to the NMBA to be registered include general registration, provisional registration, student registration and non-practising registration.
All of our active nurses and midwives are on the general register. Non-practising registration is a type of registration that is suitable for an individual who chooses to stop all nursing and/or midwifery practice but wishes – for personal rather than professional reasons – to retain a
protected nursing and/or midwifery title. Often this is a nurse or midwife who:
- has retired from nursing or midwifery practice
- is experiencing a period of prolonged illness, or
- is intending to take a long period of absence from practice.
Nurses and midwives wishing to take a period of leave (i.e. maternity leave) who are intending to return to work are advised to remain on the general register. Please note however that you must be able to maintain your CPD and recency of practice requirements.
Any nurse or midwife that transitions to non-practising registration needs to go though a process to be able to practise again. That includes lodging an application form (AGNP-40) for general registration and meet all the requirements of the following NMBA registration standards:
- criminal history
- professional indemnity insurance arrangements, and
- recency of practice.
If you the nurses or midwife does not meet the recency of practice registration standard requirement, a re-entry to practice requirement will apply.
Tips and information:
Read the renewal FAQs on the Ahpra website for helpful tips and more information on what you need to do to renew.
If you have difficulty renewing your registration online or you have a query about your registration, please contact Aphra by making a web enquiry or by calling 1300 419 495.
Mid-year Scholarships

It is time for mid-year scholarships.
Western Health has a huge variety of educational and professional development options for our nurses and midwives, and for those that would like to undertake formal educational development we have generous scholarships available.
If you are commencing a course mid-year please click on this link to apply for a post-graduate nursing courses or EN to RN transition course.
This is a fantastic opportunity to study at no cost to advance your career.
Applications close Friday 30 June 2023.
For any queries please contact Debra.Broomfield@wh.org.au or phone 0403 732 169.
Introducing mPages
Valuable feedback from nurses following the EMR Phase 1 implementation has led to the development of Nursing Admit and Nursing Manage mPages in the EMR to better support nurses with access to information.
Western Health has led the way with the development of a nursing mPage, which will be the first of its kind in Australia.
What is an mPage?
An mPage brings together information from various sources throughout the EMR to provide one comprehensive real-time view of patient information.
What are the benefits for nurses?
- Increased information sharing across all craft groups
- Decrease the ad hoc nature of the current nursing workflow
- Introduction of Dynamic Documentation (if required) in line with all other disciplines
- Streamlining of current fragmented nursing workflows to better support nursing staff including early career nurses
This tool will also allow for improved data integration, performance monitoring, data analytics, and patient safety.
3 Changes that are now available:
- Nurse Admit workflow mPage (Patient Chart)
- Nurse Manage workflow mPage (Bedside Chart)
- Dynamic Documentation for nursing – Admission & Shift Note Type
Resources
Clinical Care – Nurse Admit and Manage MPages
Training video
For more information on the Nursing Workflow mPages, please contact Kylee Ross – Kylee.Ross@wh.org.au
EMR Phase 2.1 update

There are now just ten weeks until the EMR Phase 2.1 Go-Live! It’s an exciting time for Western Health, so we have some important reminders for you:
- Those of you who were here for the EMR Phase 1 implementation in late 2018 will remember the popular Nursing and Midwifery Top 10 posters which were released weekly in a countdown to the Go-Live. These are making a return to help raise understanding and awareness prior to the EMR Phase 2.1 Go-Live. Look out for these posters which will be released weekly starting this Wednesday 3rd May
- We’ve had great feedback on the interactive EMR Phase 2.1 online WeLearn lessons, and encourage anyone who has not started their training to do so soon here
- Don’t forget, there is a helpful Q&A function in the lessons for you to ask extra questions of the Digital Health training team and to view previously asked questions and their answers
- When you have completed your training, one of the EMR Super Users for your area will be able to provide you with a login for the EMR practice environment. Practicing what you’ve learnt in training is a vital step in preparing for the Go-Live. More information on training and accessing the practice environment is available here
Keep a close eye on the Digital Health information site for all the latest information and updates on EMR Phase 2.1 as the anticipation for the July Go-Live continues to grow.
Calling all RUSONs and RUSOMs – an opportunity to be part of the EMR Go-Live!
The Digital Health team is currently seeking expressions of interest for RUSONs and RUSOMs to train as EMR Super Users and be part of the support team during the EMR Phase 2.1 Go-Live in July.
As a Supernumerary Super User, you will receive additional EMR training so that you can provide dedicated support to your colleagues during the Go-Live period by helping them with EMR workflows, navigating the EMR, performing basic trouble-shooting and, if necessary, assisting them to access further support.
This is a non-clinical role so you will not be required to participate in direct patient care or clinical decision making. If there’s anything you’re unsure of the Digital Health team will be there to help!
You will need to commit to at least three shifts per week during the Go-Live period in addition to your regular ward RUSON/M shift.
To find out more, please visit the Digital Health Information Site
Welcome to our growing Nurse Practitioners and Candidates
A Nurse Practitioner (NP) is a Registered Nurse with the experience, expertise and authority to diagnose and treat people of all ages with a variety of acute or chronic health conditions. NPs have completed additional university study at Master’s degree level and are the most senior and independent clinical nurses in our health care system. NPs work as key members of the healthcare team and collaborate with other nurses and healthcare professionals.
The title “Nurse Practitioner” can only be used by a person who has been endorsed by the Nursing and Midwifery Board of Australia.
National standards for practice ensure that Nurse Practitioners are capable of providing high quality, patient centred care. They are also capable in clinical research, education and leadership as applied to clinical care and health service development.
A Nurse Practitioner Candidate is an advanced practice nurse that is undertaking a Master’s degree and is on the journey to become a Nurse Practitioner.
Recently this innovative and vital role has grown at Western Health, with a number of new positions joining our existing Nurse Practitioner workforce, including:
- Nurse Practitioner Candidate (Dementia)
- Nurse Practitioner Candidate (Paediatric Diabetes)
- Nurse Practitioner Candidate (Critical Care Outreach)
- Nurse Practitioner Candidate (Palliative Care)
- a number of Nurse Practitioner Candidates (Emergency)
There are also a number of new Nurse Practitioners within our Renal service too.
These nurses are at the clinical peak of our profession, and we are excited that the NP role is growing at Western Health! A huge welcome to them all!
PIVC, are you sure?
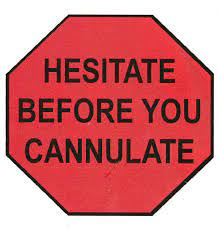
In the last 9 months Western Health experienced a steep incline in the number of peripheral intravenous cannula (PIVC) related preventable Staphylococcus aureus bacteraemia (SAB) infections. Current figures suggest 25% of patients die post contracting a SAB infection. This data is a timely reminder that we need to prevent unnecessary risk of discomfort, phlebitis and infection to our patients. So please, please, please hesitate before you cannulate. Remember these 3 key strategies:
- We want to avoid inserting unnecessary cannulas. Only insert an IVC if IV therapy is planned. We should never insert for just in case or for taking blood tests. Studies highlight around half of the PIVCs inserted in emergency are never used for any clinical purpose. Taking a moment to consider if the patient would benefit from oral analgesia/fluids or antiemetics could save their life.
- If your patients require an PIVC for clinical reasons impeccable insertion practices and maintenance care using non-touch aseptic technique and hand hygiene is essential to keeping our patients safe. Avoid the antecubital fossa (ACF) as observational studies have found that placement of PIVC in the ACF is associated with increased risk of infection and higher rates of failure especially at points of flexion. Appropriate device securement is essential and when accessing the PIVC please remember to vigorously scrub the hub for 15 seconds and then wait until dry 15-30 seconds to ensure disinfection has occurred. Professional practice standards expect HCW’s to document insertion (date, time, location and rationale) and ongoing shift assessments including during handover. Medical staff should also assess site daily with documentation with assessment of ongoing need for PIVC.
- Prompt removal when an PIVC is no longer required is a must to reduce infection risk. If there is no prescribed medication or fluid or no plan for a procedure or scan in the next 12 hours then the PIVC needs to be removed immediately. We empower our nurses to remove PIVCs if there is no documented reason for it to remain insitu. If there is any doubt, please take it out. The practice of not removing idle or redundant devices increases the risk of SAB and other organisms’ device related infections.
Evidence suggests, if we can improve our cannula care with these 3 themes, we can reduce the number of complications in our patients and make their stay more comfortable. Consider the duration of treatment and therapy agents to be given, would a longline or PICC be more suitable than multiple PIVC’s? Remember to think before you cannulate; impeccable insertion practices with aseptic technique and maintenance aseptic technique care; prompt removal. Last note, fewer PIVC insertions means more time for patient care.
Banishing Biofilm
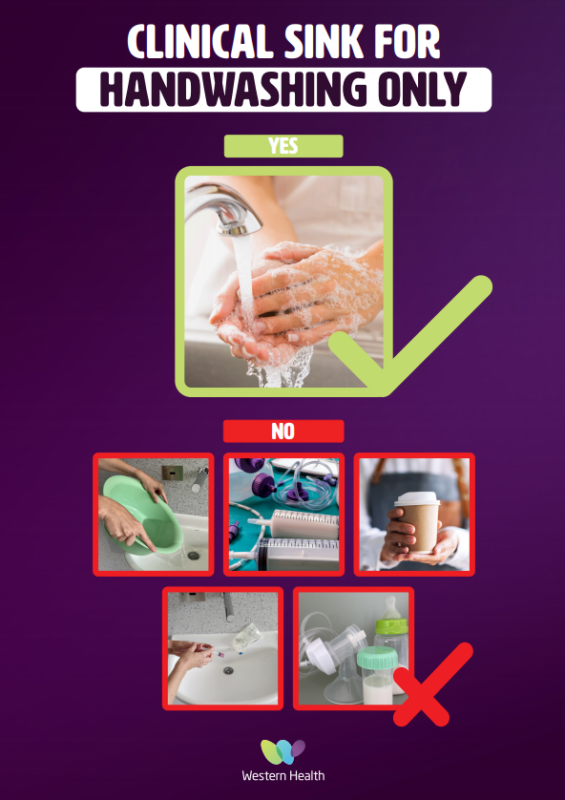
The presence of biofilm in sinks and drains has been detected throughout Western Health following an organisation wide audit. Growth has been noted in clinical and non-clinical areas. It is important that we remove the biofilm and prevent it from recurring to ensure we protect our patients and staff. In order to do this, a number of improvements are being made with the cleaning and use of sinks across all sites.
What is biofilm?
Biofilm is a slimy substance that forms in moist areas, particularly in plumbing systems. Biofilm is commonly found in hospitals and also home sinks. It’s composed of a community of bacteria enclosed in a protective matrix (a blanket like coating), which makes it hard to remove from surfaces and renders it resistant to commonly used chemical disinfectants and antibiotics.
Infections related to organisms that grow in biofilm are extremely uncommon in healthy adults including those who are pregnant. Most infections occur in hospitalised patients with indwelling invasive devices or in vulnerable groups including immune suppressed (oncology, dialysis, newborn services). Infections are caused by the bacteria that live inside biofilm and are often associated with the intensity of medical interventions these patients require.
What are we doing?
A working party has been established to direct the initial and ongoing management of biofilm in our sinks and drains. You may have noticed measures in your area including steam cleaning, replacement of sink strainers and the use of new chemical disinfectants. A trial of a new waste disposal process for IV fluids and an education campaign highlighting correct sink use is also in development. Managers will be sent individual results of their audits and be provided with instructions specific to their environment. It is important to note there is no risk to staff or patients/carers whilst steam cleaning is undertaken as the system is enclosed and prevents aerosolization of organic matter from the drains.
Protecting patients and carers – Hand hygiene is essential
It is recommended that alcohol-based hand rub is used for cleaning hands, unless they are visibly soiled. Please ensure there is always enough alcohol-based hand rub available for staff and visitors to use on entry to the ward, near sinks and in brackets on each bed.
What can you do?
We are asking for extra vigilance around hand hygiene and sterile/clean procedures from all staff to prevent transmission of pathogens from drain biofilm to patients. This can occur via splash from the sink contaminating equipment and surfaces and also on the hands of healthcare workers, medical devices and soap dispensers.
Staff can assist in preventing build-up of biofilm in clinical hand basins (CHB) by ensuring that fluids are discarded in the dirty utility room sluice or trough and must not be drained into clinical hand basins, patient bedside or bathroom sinks. This includes but is not limited to:
- IV fluids, nasogastric feeds, medications including antibiotics, TPN, dialysate fluid
- Water from patient wash bowls (contaminated with patient organisms), discarded mouthwash solutions
- Expressed Breast Milk (EBM) and baby formula
- Drinks such as tea, coffee, soft drinks or leftover food
Staff are asked to empty any leftover hot or cold beverages into kitchenette sinks and to direct visitors to these sinks if required during their visit.
Take care not to discard miscellaneous items such as IV bungs, needle caps, straws and plastic into sinks. Clinell wipes must be disposed of in bins and not flushed down toilets or sinks.
Additionally items should be stored on sinks where they can be easily splashed and contaminated.
New pharmaceutical waste disposal process is coming

Improper disposal of pharmaceutical waste can have significant financial, environmental and risk-related impacts. The current legislation mandates incineration of pharmaceutical waste, however waste in yellow sharps bins is hammer-milled. Improper disposal of pharmaceutical waste can introduce pharmaceuticals into waterways, as they cannot be sufficiently filtered by treatment plants which can affect wildlife. Due to the growing concerns regarding the improper disposal of pharmaceutical waste at Western Health, it was recognised that a new process was required to ensure compliance with legislation and address ethical and environmental concerns. As a result, a new process has been implemented in the Pharmacy Department where red pharmaceutical P22 and P64 waste bins were introduced for safe medicine disposal.
A multidisciplinary working group is currently developing the details of this new process for expansion onto our wards. Wards F1W and F2E will start to pilot the smaller P22 bins in May 2023.
These bins are designed according to Australian standards and can be ordered through FMIS. The red P22 bins (pictured above left) will replace yellow sharps bins for all medication sharps, including ampoules of Schedule 8 and Schedule 11 medicines. Red P64 bins (pictured above right) will replace the large yellow wheelie bins and will be available for all non-sharp medicines.
The bins will be placed in key areas for safe medicine disposal, such as medication rooms. Educational sessions and information posters will be provided to assist clinicians choose the correct bin.
Minimising non-slip socks

Did you know that non-slip socks are not an evidence-based fall prevention strategy?
In fact, there have been numerous studies that demonstrate they are an infectious risk, do not provide any more traction than bare feet, and often patients and/or staff will not use shoes even if available, when a patient is wearing non-slip socks. Due to variation in manufacturing, occasionally the socks can also be slippery rather than non-slip!
The use of non-slip socks at Western Health are only for patients who are unable to wear shoes, slippers or go barefoot. (e.g. swelling, wound, TEDs). Targeted, simple and specific patient and family education is evidenced as the most effective strategy to prevent falls in hospital.
Does your patient know;
- What their falls risk factors are?
- What they can do in hospital to stay safe?
Every conversation counts.
Our new Associate Professor of Nursing

It is with great excitement that we announce the appointment of Associate Professor Debra Kerr to our newly created Associate Professor role within the Western Health – Deakin University Partnership to support Pro Bodil Rasmussen and the team in furthering nurse-led research at Western Health.
Deb’s research focuses on decision support and communication with applied research to enhance the safety and quality of health care. Her areas of interest include the process of communication between nurses and patients in clinical contexts such as bedside nursing handover and in acute medical/surgical ward settings. She has also led projects in which evidence based practice and decision support tools have been developed and validated in the clinical context, particularly in the emergency setting for cardiac conditions. An area of specific focus, intranasal medical administration, has been explored as a novel and safe mode of drug delivery for naloxone and fentanyl.
Deb’s methodological approaches have predominantly focused on quantitative methods including randomised controlled trials, feasibility studies, audits and surveys. She has published over 67 peer reviewed articles and presented at international and national medical and nursing conferences. It is her aim to direct future research on the Australian National Safety and Quality Health Service Standards, in particular, the impact of communication skills training for enhancing quality and safe nursing care.
Deb will commence on 3 July 2023, however will spend some induction time at Western Health in the weeks leading up to this date. Please make Deb very welcome.
Aboriginal and Torres Strait Islander Community of Practice
Western Health’s Aboriginal Health Cultural Safety Plan 2022-2025 was developed in partnership with our Aboriginal Health Steering Committee and Aboriginal Community, and includes a strong commitment to supporting our Aboriginal and Torres Strait Islander staff.
As part of this commitment, we are inviting all of our staff who identify as Aboriginal and/or Torres Strait Islander to participate in our first Aboriginal and Torres Strait Islander Community of Practice.
The purpose of the Community of Practice is an opportunity for staff to get together and to let the organisation know, in a culturally safe space, what works well at Western Health and what improvements could be made. It is also an opportunity for staff to get to know each other and help inform ways we can better attract, support and retain staff that identify as Aboriginal and/or Torres Strait Islander.
The first Community of Practice will be held:
Date: Monday 15th May
Time: 11 am – 1 pm
Venue: Club Italia, 128 – 132 Furlong Road, St Albans
If you identify as Aboriginal and/or Torres Strait Islander and would like to attend please contact Tanya Druce on tanya.druce@wh.org.au or 0403 947 775.
If you would like to update your cultural details on Western Health systems, please complete an Update Personal Details form which can be found on the People and Culture forms page under ‘P’ and then sent through to peopleservicesoperations@wh.org.au.
For any staff who want to learn more about Aboriginal culture and supporting our staff and patients who identify, please access the Aboriginal Cultural Awareness training on WeLearn.
New Victorian Chief Nursing & Midwifery Officer

Safer Care Victoria recently announced that Karrie Long has been appointed as Victoria’s new Chief Nurse and Midwifery Officer (CNMO). Karrie is a visionary nursing leader with over 15 years’ experience driving health delivery innovation to ensure safer and more effective patient care. This year, she became an inaugural recipient of the Florence Nightingale Foundation’s Dame Yvonne Moores Global Leadership Scholarship.
In her role as CNMO, Karrie will provide professional leadership, advice, and direction to the sector drawing on a unique set of skills acquired across all aspects and levels of nursing, including regional and metropolitan health settings and academia. Karrie brings with her an expansive knowledge of Victoria’s public health system gained through her previous roles as a clinician in intensive care and in education, digital health, research, and senior leadership, including the Director of Nursing Research and Interim Chief Nursing Officer at the Royal Melbourne Hospital. Karrie has a Graduate Diploma in Advanced Clinical Nursing (Rural Critical Care) and a Master of Public Health.
Karrie spent her childhood in Papua New Guinea, which has been a strong driving force behind her career in health and where she can be of service, particularly to vulnerable and voiceless populations. She demonstrates a real passion for digital health, having designed and implemented Telehealth at the Royal Melbourne Hospital. This was informed and driven by a career of nearly 20 years of practice in regional Victoria, where she saw the need to better connect, improve and innovate health for all Victorians.
Karrie started in her new role with Safer Care Victoria on Thursday 20 April 2023.
Flu and COVID Vax'd - Stronger Together!

The Western Health Staff Influenza Prevention program offers a free vaccine to every member of staff in a bid to keep our Health Service influenza safe.
Additionally, this year maintaining up-to-date vaccination against COVID continues to be an integral defence to protect us against this disease. Boosters are important to maintain this protection.
This year staff will be able to receive both the influenza vaccine, and if they wish a COVID booster vaccine at the same time.
The 2023 Influenza and COVID Immunisation Program was recently launched across all Western Health sites.
The annual influenza vaccine is mandatory for all Category A and B healthcare workers, which includes the vast majority of nurses and midwives:
- These are healthcare workers who have direct physical contact with patients, clients, deceased persons or body parts, blood, body substances, infectious material or surfaces or equipment that might contain these OR
- Contact that might allow respiratory infections to be acquired or transmitted, which includes workers with prolonged face-to-face contact with patients or clients or where their normal work is in a clinical area.
We encourage Category C staff to receive the influenza vaccination to protect themselves and their loved ones.
The COVID booster is not mandatory, but highly recommended. For those of you who want to get in early, as of this Monday the 17th we will be opening a COVID Vaccination pop up clinic at Footscray Hospital, front foyer for walk ins, no appointments required.
Staff from all areas are invited to attend any of our launch dates above, as well as fixed or roaming immunisation clinics thereafter. Fixed and roaming clinic dates will be publicised and will be made available on the Western Health Infection Prevention intranet site.
Please be reminded that:
- Staff must have their Medicare card or IHI number in order to be vaccinated.
- If staff have been vaccinated at another hospital, by a GP or elsewhere, please complete a quick Redcap survey click on link access: Influenza Immunisation Survey and attach your immunisation certificate and/or provide us with consent for Western Health Immunisation staff to check your Australian Immunisation Record (AIR)
- All staff who decline the influenza vaccination (including Category A, B and C staff) must complete their declaration on Redcap. Please follow this link to access: Influenza Immunisation Survey
- Staff who have one of the 3 medical exemptions to receiving the influenza vaccine MUST complete a Redcap survey and attach a medical certificate from a medical practitioner. Please click on the link to access: Influenza Immunisation Survey.
- Managers will need to monitor their MAP report and follow up on Category A and B staff uptake of influenza vaccination and any staff declinations.
Supporting Aboriginal and Torres Strait Islander self-determination
Western Health’s Board of Directors has issued the following statement in support of First Nations self-determination, drafted by our Wilim Berrbang team in consultation with Aboriginal staff and members of the Aboriginal community.
The Western Health Board of Directors acknowledges the Traditional Custodians on the land on which our sites stand. We pay our respects to Elders past, present and emerging. We are committed to healing of country, working towards equity in health outcomes and the ongoing journey of reconciliation.
The Uluru Statement from the Heart calls for a First Nations voice be enshrined into the Constitution of Australia, a step towards self-determination and the real ability for First Nations people to influence decision making when the decision will affect them.
At Western Health, we are committed to ensuring First Nations people have the right to self-determination during their healthcare journey. We firmly believe in the guiding principle of self-determination, where Aboriginal and Torres Strait Islander staff, people and communities are empowered to own, direct and make decisions in designing, delivering and evaluating Aboriginal health policies, programs and initiatives.
The road to self-determination and the Uluru Statement from the Heart has not been an easy journey for many Aboriginal and Torres Strait Islander people. It has been a constant fight for justice, truth-telling and for self-determination. Western Health pay our respects to those who have fought and those who continue to fight for these rights.
Western Health is thoroughly committed to working in partnership with our Aboriginal and Torres Strait Islander staff, volunteers and patients and families. We also recognise that Aboriginal and Torres Strait Islander people are culturally diverse and have a range of life experiences, opinions and perspectives. It is vital every Australian who is eligible to vote considers the weight and importance of the question fully and informs themselves of the history and issues that sit behind the referendum. We are sure that differences of opinion can be handled with respect and integrity. We encourage everyone who can to walk alongside our Aboriginal and Torres Strait Islander communities through this part of their journey, towards long-lasting change.
Nurse-led research team receives 2 prestigious MRFF grants

The Medical Research Future Fund (MRFF) is a prestigious research fund set up by the Australian Government to fund healthcare research projects that transform healthcare to improve lives, build the economy and contribute to health system sustainability. The grants are extremely competitive, and in the past nurse-led and midwife-led research projects have rarely been successful.
This year the Western Health-Deakin University Partnership have been successful in receiving 2 MRFF grants, which is phenomenal!
- Western Health in conjunction with University of Melbourne, South Western Sydney Local Health District and University of Sydney have been successful in their recent MRFF grant application to research the Natural Helper approach to culturally responsive healthcare.
- In addition, Prof Bodil Rasmussen has been successful in a joint MRFF grant to research Translating heart failure guidelines into practice: an RCT of a Nurse Practitioner service.
This is an amazing achievement, congratulations to our research teams.
Our Nursing Research team recognised

On 4 April 2023 the Western Health and Deakin University partnership took out 3 of the 6 awards on offer at the inaugural Deakin University Faculty of Health Partnership Awards event.
The partnership won the award for the following categories:
- Middle career research award: Sara Holton, Karyn Winter and Professor Bodil Rasmussen took out this award for their work into the impact of the COVID pandemic on health professionals and undergraduate students
- Health Service Partnership: Danielle Hitch (Research and Translation Lead, Allied Health), Sara Holton and Professor Bodil Rasmussen took out this award for their collaborative research into the impact of Long COVID on patients
- Partnership in Practice: Veronica Graham from the Western Public Health Unit, Deakin University and Department of Health took out this award for their research into adaption of the evidence based program INFANT within diverse and economically disadvantaged communities.
Overall winner from all categories was:
- Partnership in Practice: Veronica Graham from the Western Public Health Unit, Deakin University and Department of Health, took out this award for their research into adaption of the evidence based program INFANT within diverse and economically disadvantaged communities supporting new parents.
Congratulations to all of the Western Health staff and Deakin University staff involved in these projects, and wonderful that they have been acknowledged with through these awards.
Benchmarking Best Care
The latest benchmark reports from the Health Roundtable that go up to December 2022 have recently been released, that show how our delivery of Best Care compares to other health services across Australasia.
The reports below shows a summary, as well as a 4 year trend in all hospital acquired complications.
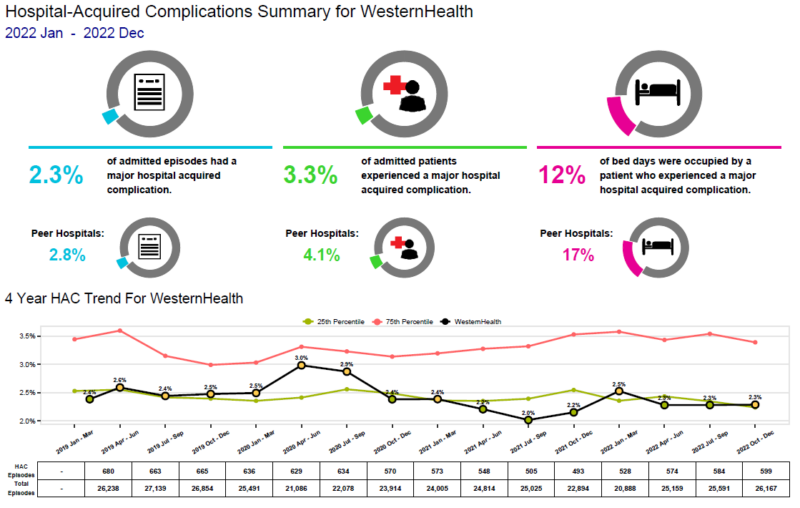
For Western Health as a whole:
2.3% of our admitted episodes had a major hospital acquired complication (compared to 2.8% at our peers),
3.3% of admitted patients experienced a major hospital acquired complication (compared to 4.1% at our peers).
12% of our bed-days were occupied by a patient who experienced a major hospital acquired complcation (compared to 17% at our peers).
Pleasingly our rate of hospital acquired complications rate over the past 4 years has been progressively dropping – and predominantly green when compared to our peers.
In future months we will go into detail for some of the nurse and midwife performance indicators.
Educational Opportunities

Resuscitation Mandatory Competencies:
Sessions have recommenced. In the first instance, you can arrange an assessment with your local instructor or educator. Resus educators are contacting managers to arrange local sessions for individual teams. Dedicated sessions for Bank and Pool Staff along with sessions for Nursing and Medical staff are available on Welearn. You can locate sessions by clicking on this link: Course: Basic Life Support (BLS) (wh.org.au)
Invasive Lines & Cannulation:
Dates for Bank-Pool Nursing staff, Ward Nursing staff, Radiology, and Medical staff available soon.
Adult Deteriorating Patient (non-obstetric):
Learning how to recognise and escalate patient deterioration is now here at Western Health. The Education and Learning Department have developed a new and improved Welearn course, designed to guide and support early recognition and escalation for a patient deteriorating within WH. I encourage all staff to complete the course and once completed, book in for a face-to-face study day to further improve and practice newly developed skills.
Fisher and Paykel Respiratory Support training:
RSVP to: education.australia@fphcare.com.au
- Infant & Paediatric Respiratory Support: Wednesday 10 May 2023 – WCHRE Auditorium: 9.00am to 3.00pm
- Adult Respiratory Support: Friday 14 July 2023 – WCHRE Auditorium: 9.00am to 3.00pm
- Infant Respiratory Support: Friday 1 September 2023 – WCHRE Auditorium: 9.00am to 3.00pm
- Adult & Paediatric Respiratory Support: Wednesday 4 October 2023 – WCHRE Lecture Theatre: 9.00am to 1.00pm
Education and Learning upcoming events:
- 20/03/2023: VAC Therapy Study Day
- 21/03/2023: CVAD Workshop
- 23/03/2023: Infection Prevention Study Day
- 27/03/2023: Tracheostomy Study Day
- 29/03/2023: Bookings are open for PIVC at Sunshine via the Welearn Module
- 04/04/2023: Heart Failure Study Day
- 14/04/2023: ALS1 training
- 20/04/2023: Microsoft Excel Introduction
- 20/04/2023: Microsoft Excel Intermediate
- 21/04/2023: Mental Health First Aid
- 26/04/2023: Night Duty: Deteriorating Patient
- 28/04/2023: Mental Health First Aid
- 03/05/2023: Cognitive Study Day
- 18/05/2023: Renal Study Day
- 19/05/2023: Mental Health First Aid
- 26/05/2023: Mental Health First Aid
- 30/05/2023: Bank/Pool Study Day
- 14/07/2023: Adult Respiratory Support (External enrolment)
- 05/09/2023: Cognitive Study Day
- 21/09/2023: Infection Prevention Study Day
- 27/10/2023: Mental Health First Aid
- 03/11/2023: Mental Health First Aid
More courses click here: Courses and Inservices (westernhealth.org.au)
Course Enrolment/Inquiries:
- WeLearn Helpdesk Email: welearn@wh.org.au
- WeLearn Enrolment link: welearn@wh.org.au
Emerging Evidence
The Western Health Library Service is a great source for locating the latest nursing and midwifery related evidence-based practice and research.
Latest articles of interest:
- Feasibility and acceptability of an online guided self-determination program to improve diabetes self-management in young adults. Digital Health. 2023: March Full Text Western Health Author
- Experiences and information needs of women who become pregnant after bariatric surgery: An interpretive descriptive qualitative study. Midwifery. 2023: March Full Text Western Health Author
- Outcome of reduction of paediatric forearm fracture by emergency department clinicians. Emergency Medicine Australasia. 2023: April Full Text Western Health Author
- Nurse practitioners treating ankle and foot injuries using the Ottawa Ankle Rules: a comparative study in the emergency department. Australasian Emergency Nursing Journal. 2013: August Request Article Western Health Author
- Accurate identification and documentation of First Nations women and babies attending maternity services: How can we ‘close the gap’ if we can’t get this right? Australian &New Zealand Journal of Obstetrics & Gynaecology. 2023: April Full Text Western Health Author
NSQHS Standards – Live Literature Searches (Support for Accreditation):
These searches are primarily aimed at staff working in Australian hospitals who wish to find evidence to support best practice in line with Australian National Safety and Quality Health Service Standards. They are provided through a joint initiative of Health Libraries Australia (HLA) and Health Libraries Inc. (HLI) and have been adapted and expanded to reflect NSQHS 2nd edition. The searches are provided in PubMed, as a platform that is freely available and a source of quality health evidence.
Full Text Options:
- Open access content is sometimes available directly from PubMed
- Install the Western Health Library’s LibKey Nomad browser extension. PDFs will appear in the PubMed results page.
- Use the Library’s Custom PubMed Link in another tab before using the links on the page.
- Use one of the other options available on the library’s Locating Journal Articles
- If not available from the above, you can request the article from the library.
Accessing the Library at Work:
All eligible staff can access electronic library resources from any networked PC or device connected to
Wi-Fi network without the need to login.
Accessing the Library Remotely (offsite access):
- When accessing electronic resources through the library website from offsite you will automatically be asked to enter your library membership number and surname.
- Library Membership is free and can be completed online.Please email the library if you experience issues when registering (e.g. error messages).
For more information please contact the Western Health library team

