Published on 1 March 2022
Edition 52: March 2022
-
Helpful contacts
Employee Assistance Program: 1800 099 444
Nurse & Midwife Support: 1800 667 877
Nurse & Midwife Health Program:
03 9415 7551 or 1800 888 236 -
Upcoming Dates
March 2022
4 Fatigue Management session (2:30pm)
7 Manager Support Program (2:30pm)
9 Manager Support Program (11:30am)
14 Labour Day
16 Manager Support Program (11:30am)
21 MACH Future Leader Fellowship program applications close (9am)
22 Manager Support Program (2:30pm)
23 Manager Support Program (11:30am)
28 Manager Support Program (2:30pm)
29 Deadline for Mandatory Third COVID vaccine dose (for staff eligible after 12 January)
30 Manager Support Program (11:30am)April 2022
13 Nursing & Midwifery Grand Round (2:30pm)
15 Good Friday Public Holiday
18 Easter Monday Public Holiday
25 ANZAC Day
26 Riskman 2 go live
27 Falls Improvement Plan launch (Grand Round) -
The Nursing & Midwifery Executive
Adjunct Professor Shane Crowe
Executive Director of Nursing & Midwifery
Phone: 8345 1463
Email: shane.crowe@wh.org.auAllison Lamb
Acting Director of Nursing & Midwifery, Williamstown Hospital
Division: Aged Cancer and Continuing Care
Phone: 0421 950 501
Email: allison.lamb@wh.org.auProfessor Bodil Rasmussen
Chair of Nursing, Deakin University/Western Health
Phone: 8395 8163
Email: bodil.rasmussen@wh.org.auDoug Mill
Director of Nursing & Midwifery
Divisions: Chronic & Complex Care, Drug Health
Phone: 8345 1916
Email: douglas.mill@wh.orh.auHelen Sinnott
Director of Nursing & Midwifery, Sunshine
Divisions: Women’s & Children’s, Clinical Support & Specialist Clinics
Phone: 0435 962 716
Email: helen.sinnott@wh.org.auJo Mapes
Director of Nursing & Midwifery, Footscray Hospital
Division: Perioperative and Critical Care
Phone: 0423 302 337
Email: joanne.mapes@wh.org.auKate Renzenbrink
Director of Nursing & Midwifery Informatics (CNMIO)
Phone: 0425 772 324
Email: kate.renzenbrink@wh.org.auProfessor Linda Sweet
Chair of Midwifery, Deakin University/Western Health
Phone: 8395 1178
Email: linda.sweet@wh.org.auLisa Gatzonis
Director of Nursing & Midwifery Workforce
Phone: 9393 0127
Email: lisa.gatzonis@wh.org.auMandy Cullen
Acting Director of Nursing, Melton Health
Phone: 0413 867 065
Email: MandyCu@djhs.org.auNicole Davies
Director of Nursing & Midwifery, Sunbury Day Hospital
Division: Emergency, Medicine & Access, Western PHU
Phone: 9732 8630
Email: nicole.davies@wh.org.auRohan Vaughan
Director of Nursing, Bacchus March Hospital
Phone: 0434 365 769
Email: rohan.vaughan@wh.org.auSue Sweeney
Director of Midwifery Practice
Phone: 0466 801 447
Email: sue.sweeney@wh.org.auAssociate Professor Tony McGillion
Director of Nursing & Midwifery (Inspiring Innovation)
Phone: 0466 925 108
Email: tony.mcgillion@wh.org.au
From Shane

I’m sure that you are all as pleased as I am that things feel much more ‘normal’ over the past couple of weeks. Our workforce status is looking significantly improved with all areas now back at usual staffing levels. In fact, with our RUSONs and RUSOMs we are at enhanced staffing levels. We have moved all redeployed staff back to their normal locations, and elective surgery recommenced on 28 February at Footscray Hospital in limited numbers and at Bacchus Marsh Hospital. Elective surgery will recommence at Williamstown and Sunbury over the coming weeks. So many members of our community have had access to treatment and care delayed due to COVID, so having this recommence is such an important step.
You should all feel enormously proud that the overall safety and quality of nursing and midwifery care that has been provided has not deteriorated over the incredibly busy COVID peaks. In fact, from the data that we have available to us at this time, it appears that in many areas the improvements to which you have all been contributing have continued despite the data showing us that the acuity and complexity had significantly increased. Your dedication to providing Best Care to our community despite adversity is humbling.
Over the past weeks we have had many debrief sessions running to support our nurses and midwives, as well as sessions on managing fatigue. Many of these sessions were facilitate by external experts. I want to share with you unsolicited comments that I received by the CEO of the Nursing & Midwifery Health Program Victoria on his observations of Western Health nurses and midwives: “I have – during every one of the groups I have facilitated at Western Health – found everyone to be incredibly focused, patient and positive, in spite of the obvious challenges they continue to confront…. I have also been struck – during every forum – by the quality of person you have managing the respective departments. They have each been a joy to liaise with and importantly they care for their workforce AND their workforce appears to care for them. This is truly remarkable as it’s not something I always see during my incursions to health services.” This is high praise indeed, and a testament to the Western Health way – something that we need to ensure we continue to nurture and not take for granted.
A huge welcome to our first group of new Graduates for 2022 that have recently commenced on our wards and departments. It is wonderful to have you join Western Health, and I am sure that you will find that our teams will ensure that you get settled in quickly and are supported to make a successful transition from student to healthcare professional. This is a challenging leap for everyone, however I am confident that our Grad+ program and our positive workplace culture will provide you with the support needed to ensure that you thrive. I hope that this is the start of a happy and long career here at Western Health.
The Fair Work Commission recently approved the Nurses and Midwives Enterprise Agreement 2020-24, and Western Health has already been busy implementing most of the new requirements. We will continue to implement the remaining new elements over the coming months.
Finally as our workforce thankfully returns to normal, I’m sure that most of you have seen the benefits and are appreciating the positive impact that team-based care provides to our patients/women – as well as helping to ensure that workloads are achievable for our nurses and midwives. We are team-based professions, and are stronger when we work together. I encourage you all to continue to work within your teams to optimise the way you all work together, using the principles of delegation and supervision to spread the workload and decrease any missed elements of care. Let’s continue to work together to provide the Best Care possible and look after each other.
Shane Crowe
Executive Director, Nursing & Midwifery
Welcome to our new Grads

This year Western Health is welcoming 307 new nursing and midwifery graduates to our team, and to the best professions in the world! A very warm welcome to all of our new colleagues to Western Health.
The first intake of eager graduates started early on 7 February, with 58 more commencing in March and a further 23 in June.
Our new graduates are commencing Year 1 of our new Grad+ program, which is a 2 year program which includes 4 rotations, with the second year including more rotations into specialty areas. The program also includes 2 free Western Health post-graduate subjects that are accredited with 5 universities focusing on advanced clinical assessment, pathophysiology and clinical leadership.
The program has been specifically designed to offer benefits to our early career nurses and midwives that include:
- Offer an entry to practice program that provides wider experience to different clinical specialties, to create well-rounded nurses and midwives with diverse experience in their early career years.
- Support our nurses and midwives to be able to have broader experiences and options available to them prior to choosing their preferred specialty
- Embed a culture of life-long learning through supporting the continuation of formal education into the early career years
- Make post-graduate education more accessible and affordable for our nurses and midwives
- Increase participation rates in post-graduate education, by offering 2 free subjects as part of their early career years.
- Enhance Western Health’s status of an employer of choice for newly graduated nurses and midwives.
We know that you will make your new colleagues feel welcome as they join the team.
Fair Work Commission approved new Enterprise Agreement

On Wednesday 16 February 2022 the Fair Work Commission approved the Nurses and Midwives (Victorian Public Health Sector) (Single Interest Employers) Enterprise Agreement 2020-2024.
The Agreement is available to be viewed on our Workforce page and came into effect on 23 February 2022.
Western Health has already been implementing key components of the new Agreement. Now that the new Agreement has been formally approved we will be methodically working through an implementation process to ensure that all aspects are in place. This implementation process includes regular meetings of our Workplace Implementation Committee, which has representation from both Western Health and ANMF.
Our nurses and midwives will be kept informed of any changes that affect you directly as we go through the implementation process.
Final mandatory third dose COVID Vaccine deadline rapidly approaching
A reminder that the first deadline for the mandatory third dose of a COVID vaccine is rapidly approaching. For healthcare workers who become eligible to receive the COVID Vaccination booster after 12 January 2022 must have received their third dose by 29 March 2022.
The mandatory vaccination requirement will not apply to workers who have a valid medical exemption.
It is vital that all staff have a plan in place by their due date to either:
- Have the third dose at a Western Health vaccination site, or
- Supply evidence of having received the third dose elsewhere, or
- Supply evidence of having a medical exemption.
Western Health will have evidence of dose dates for all vaccinations administered at a Western Health vaccination centre. No action is required if you have received your third dose at a Western Health operated site.
If you have received your third dose at a location other that a Western Health vaccination site or have a medical exemption, you must complete this survey to ensure that Western Health has this evidence to update our records.
Extended Leave and Non-practising Registration

Every year Western Health has a large number of nurses and midwives go on some extended leave. Often this is for something like maternity leave or long service leave, where they fully intend to return to work following their leave.
Occasionally some of our nurses or midwives have fallen into the trap of applying for non-practicing registration during their leave, which has impaired their ease of returning to work.
The Nursing and Midwifery Board of Australia (NMBA) regulates the practice of nursing and midwifery in Australia, and one of its key roles is to protect the public. The NMBA does this by developing registration standards, professional codes, guidelines and standards for practice which together establish the requirements for the professional and safe practice of nurses and midwives in Australia.
The types of registration available to nurses and midwives who apply to the NMBA to be registered include general registration, provisional registration, student registration and non-practising registration.
All of our active nurses and midwives are on the general register. Non-practising registration is a type of registration that is suitable for an individual who chooses to stop all nursing and/or midwifery practice but wishes – for personal rather than professional reasons – to retain a
protected nursing and/or midwifery title. Often this is a nurse or midwife who:
- has retired from nursing or midwifery practice
- is experiencing a period of prolonged illness, or
- is intending to take a long period of absence from practice.
Nurses and midwives wishing to take a period of leave (i.e. maternity leave) who are intending to return to work are advised to remain on the general register. Please note however that you must be able to maintain your CPD and recency of practice requirements.
Any nurse or midwife that transitions to non-practising registration needs to go though a process to be able to practise again. That includes lodging an application form (AGNP-40) for general registration and meet all the requirements of the following NMBA registration standards:
- criminal history
- professional indemnity insurance arrangements, and
- recency of practice.
If you the nurses or midwife does not meet the recency of practice registration standard requirement, a re-entry to practice requirement ill apply.
It's raining RUSON/Ms

Western Health is further expanding our use of Registered Undergraduate Student of Nursing/Midwifery (RUSON/M) roles following a successful 12-month pilot on the initial 6 wards. The utilisation of these roles significantly grew over 2021 during the COVID Surge period – and were instrumental in supporting our nurses and midwives during this challenging period and allowing our teams to continue to provide Best Care.
Key findings from the initial RUSON pilot includes:
- The RUSON role enabled others to better manage acuity and access demands
- The RUSON role released more time to spend with patients and was viewed as an essential role by peers
- The RUSON role contributed to risk prevention and could be described as the ‘gatekeeper’ of the patient experience through their engagement and presence
To further support our wards, additional second year RUSONs are currently being employed to replace the recently graduated RUSONs.
To enhance the program, this year we will be focusing on:
- Enhancing our governance structures, ensuring the Nurse Unit Managers have consistent and standard tools to maximise the benefits of the RUSON role
- Increasing the Nursing and Midwifery Directorate support for this key role by facilitating the success of our RUSONs ‘through’ appropriate support of our Nurse Unit Managers
- Maximising the RUSON ‘pipeline’ to funnel into Fellowship Programs and graduate employment at Western Health, optimising their gained knowledge of systems and processes. We will provide mentoring for them to encourage them to successfully transition through these time points, to help them become more confident and proficient in their early career years.
To all of our RUSON/Ms we say a sincere thank you for everything that you do to support Best Care and ensuring a good experience for our patients. We look forward to continuing to work with you into the future, and welcoming new RUSON/Ms on board to support additional teams.
Eve App to enhance antenatal care

In March our maternity team at Western Health are launching an innovative digital solution that will enable pregnant women and new mothers to have access to information and assistance when they need it.
The Eve App is a mobile application designed to enhance the pregnancy and parenting experience for expectant and new mums in the West by providing them with access to evidence based information relating to pregnancy, birthing and early parenting.
The implementation of the Eve App aims to improve women’s involvement in their own care and improve the quality and timeliness of the information they were seeking regarding pregnancy, birthing and early parenting.
The COVID-19 pandemic has led to us needing to look for other ways for women to engage with us, given restrictions to face to face antenatal care. Many women use Google and commercially available apps or ask on forums when they are seeking information – almost everyone has a smartphone, however unfortunately this often results in misinformation, scaremongering and even sometimes online bullying.
When women book in to have their baby at Western Health, they will receive a SMS inviting them to download the application. This will be linked to their specific booking and their own medical record and will have bank-level encryption to ensure privacy is maintained. Women will receive weekly updates about how their body is changing and baby is growing and have new articles that are relevant to their stage of pregnancy/parenting. They can also search for specific articles or topics that they are interested in.
The Eve app has practical content such including:
- Serious pregnancy symptoms you should never ignore
- What is fetal monitoring?
- Tired cues
- Expressing breast milk
- Babies first 24 hours
- Alcohol, smoking, drugs and medications when breastfeeding.
The educational content is initially available in English, however Western Health will be working collaboratively with the company and other health services to make resources available in other languages in the future.
Point Cook Community Hospital land purchased

The Minister for Health recently announced that the land has been purchase for the planned new Point Cook Community Hospital to be built. Located at 140 Dunnings Road, Point Cook, the site is next to the Point Cook Shopping Centre, close to public transport and is accessible from the freeway.
Once constucted this new small public hospital, which will be operated by Western Health, will provide a range of integrated community health and specialist services. It will give the local community greater access to health services, closer to home.
The project will help take pressure off Werribee Mercy, Footscray, and Sunshine hospitals. This assists major hospitals to focus on critical care, emergencies and more complex surgeries and procedures.
Construction is expected to start in 2022 and be completed in 2024.
Riskman 2 coming soon
To meet new Department of Health reporting requirements, our Riskman Incident Register will be upgraded on 26 April 2022. Please note: Bacchus Marsh/Melton run a separate Riskman system and this will also be upgraded, but closer to the end of June 2022.
The upgraded Riskman will be more user friendly and intuitive than our existing register.
Changes you will notice in the upgraded Riskman are as follows:
- A new look with colours and a more user-friendly layout
- The ‘Notification Type’ field has been replaced with a ‘The Event relates to a’ (drop down) field
- A new way to select incident classifications / types of events
- A functionality has been added to the Medication section where you will be prompted to select a medication name on the basis of your search
- Slight wording changes to severity rating headings and the inclusion of links to definitions
- A new read only field to display that incident details have been transmitted to the Department of Health
To support staff understand the updated layout of the new Riskman and the key changes that have been added to this, the following training resources have been developed:
- Zoom Training Sessions – between 16 March – 22 April, 60 minute zoom training sessions will be held at 11am and 2pm on Mondays, Wednesdays and Fridays (except on public holidays). Find out more about these sessions by clicking here
Additional sessions can be run by agreement – contact WHS-RiskmanHelpdesk@wh.org.au
It is highly recommended staff watch the video noted below before attending zoom training sessions. A recording of the zoom training session will be made available for staff working nights and weekends.
- WeLearn Training video – 30 minutes in duration. This video introduces the Upgraded Incident Register and demonstrates the key changes staff will see on the new register. Click here to access the WeLearn Training video.
- Cheat sheet – A quick reference guide includes screenshots and details of the key changes in the new incident register. The QRG can be accessed through the Best Care Microsite
- Riskman helpdesk – contact the helpdesk at WHS-RiskmanHelpdesk@wh.org.au or talk to a WH Quality Partner
What to expect on ‘Go Live’ day
- Riskman will be accessible as usual and staff login details will remain unchanged
- Once logged in staff will access the upgraded Riskman incident register
- Staff will be able to access and manage incidents entered prior to the Riskman Upgrade
Duty of Candour requirements to be introduced this year

Patients who are seriously harmed in hospitals will receive a genuine apology, understand what happened and why, and be part of future improvements – thanks to legislative amendments passed by Parliament on 23 February 2022.
Amendments to the Health Services Act 1988 will improve transparency in Victoria’s health system, by encouraging staff to report adverse outcomes, and talk openly with patients if something goes wrong.
For the first time in Australia, from November 2022 public and private hospitals will be required to:
- apologise to any person seriously harmed while receiving care
- explain what went wrong
- describe what action will be taken and improvements put in place.
Building on the Australian Open Disclosure Framework, the amendments also introduce legal protections around health service apologies and clinical incident reviews. This means that any apologies and internal reports cannot be used in a court of law but will be available to patients or their family members and carers.
Safer Care Victoria will develop guidelines, training and resources to help health services prepare and implement the changes.
New departments supporting flow at Sunshine
On Monday, 7 March, Rapid Assessment and Discharge Unit (RADU) will open at 2G Sunshine, which will be a 24-bed unit that will support the flow of general medicine patients for SHED to the ward.
Additionally a Transit Lounge at Sunshine Hospital recently re-opened in a trial basis. To arrange transfer of your patients to the Transit Lounge, please call the Transit Lounge on 0421 995 959 to make referrals to the lounge. There is a dedicated Discharge Navigator role that will work to identify patients across all wards who are suitable for transfer to the Transit Lounge. This role will also support identification of patients who can be discharged home with support from Western@Home services, supporting timely discharge and access to the right services.
The new Transit Lounge:
- Features 9 recliner chairs and bed availability, with capability to grow and flex to meet demand from the hospital
- Operates seven days, 0800 – 1830 hours
- The Transit Lounge Team, which includes PSAs, nurses and RUSONs, will take a verbal handover over the phone and collect the patient from the ward. No written handover required.
Eligibility Criteria has been expanded to patients:
- discharging to home; residential aged care facility; awaiting transfer to subacute ward or another hospital.
- Awaiting medications, discharge prescription, or medical certificate
- Requiring “last dose of medications” (e.g. IV antibiotics, insulin), medical imaging or pathology results prior to discharge
- Awaiting discharge review from medical officer or allied health
- Awaiting transport or pick-up
- Patient discharging from the Sunshine Emergency department requiring Transit Lounge support
Exclusion Criteria for the Transit Lounge includes any patient that:
- is medically unstable;
- is displaying significant Behaviours of Concern (BOC score >2);
- requires infection prevention contact or droplet precautions.
Sunshine Fast Track now open
On Monday 21 February the new Adult Fast Track area of the Sunshine Hospital Emergency Department (SHED) commenced operating, which is a significant milestone in the expansion project .
The aim of the Fast Track model is to improve the patient experience for low-acuity patients, while improving access and flow through the Emergency Department.
The new Adult Fast Track is located on Level One of the SHED expansion and has 15 points of care for patients presenting with less serious illnesses and injuries. Care of patients in Fast Track is provided by a multidisciplinary team, ensuring timely assessment, treatment and discharge. The Fast Track area also includes a treatment room, plaster room, and two digital imaging suites (X-ray and ultrasound).
The hours of operation are 0800-2330, 7 days a week. Outside of these hours, patients will be streamed to the Short Stay Unit or the Emergency Department.
Significant recruitment has been undertaken to staff these additional points of care in Fast Track, and well done to everyone involved. Th team’s focus now moves to operationalising the Behavioural Assessment Unit.
Further information and resources are available to you and your teams via unitED.
Maternal Child Health Nurses answering the call
Western Health has been collaboratively working with Brimbank City Council, Hobsons Bay City Council and Hume City Council to allow some of their Maternal Child Health Nurses to be freed up to allow them to support our maternity services during February and March 2022.
In response to maternity and neonatal health service needs due to the COVID-19 pandemic, Western Health and the Councils share a common objective to achieve the best possible outcomes for the provision of midwifery, neonatal and Maternal and Child Health (MCH) services for women, infants and their families throughout the western metropolitan region.
As Western Health has been impacted by staff shortages within our maternity services – together with an incredibly busy March, we liaised with Safer Care Victoria and Councils to implement a short-term surge model to support our midwives. In this model Maternal Child Health nurses will undertake the role of the midwife in domiciliary care for a fixed term, allowing our hospital-based midwives to remain in the acute setting and provide care to women and infants during the antenatal, intrapartum and early postnatal periods prioritising the most vulnerable women and infants.
We welcome our Maternal Child Health colleagues to Western Health, and sincerely thank them and the Councils for their support during these challenging times.
Join a study about the impact of P2/N95 masks on nurses during COVID-19
 Anie Edward, Infection Prevention Nurse Consultant, was awarded the 2021 Western Health Mavis Mitchell Scholarship to investigate nurses’ experiences of using of P2/N95 masks during the COVID- 19 pandemic. Anie now has Ethics approval for her study and would like to invite eligible nurses to participate:
Anie Edward, Infection Prevention Nurse Consultant, was awarded the 2021 Western Health Mavis Mitchell Scholarship to investigate nurses’ experiences of using of P2/N95 masks during the COVID- 19 pandemic. Anie now has Ethics approval for her study and would like to invite eligible nurses to participate:
- Are you a registered nurse or enrolled nurse at Footscray or Sunshine Hospital?
- Do/did you work in a COVID-19 designated ward?
- Have you experienced facial skin reactions or facial pressure injuries due to wearing P2/N95 masks?
- Have you cared for a COVID-19 patient whilst having facial skin reactions or facial pressure injuries?
If you have answered yes to 3 or more of the questions, then you are eligible to participate in this study. If you are interested, please contact Anie Edward (Anie.edward@wh.org.au) about participating in an interview.
Everyone who participates in an interview will receive a coffee voucher and will go in the draw to win one of two $50 gift cards.
Thank you for your interest in the study and we hope you agree to participate.
Simplified Nursing Student Assessment update

The simplified version of the Australian Nursing Standards Assessment tool (ANSAT) has been in use at Western Health during February and March to document student assessments. This was implemented in recognition of the impact that COVID surge has had on health services. The Australian Nursing & Midwifery Accreditation Council (ANMAC) has approved this simplified tool being used for nursing students until 20 March 2022.
The principles for application of the modified tool are:
- Written feedback will be provided under each Standard by exception, however must be completed if/when a student scores 1 or 2 in any assessable item.
- A formative assessment is only required to be undertaken on placements greater than 2 weeks in length.
- Regardless of length of clinical placement a formative assessment is undertaken on students that are repeating a placement or had prior issues on placement as advised by the education provider.
Western Health’s Centre for Education can be contacted for any support or further information about the new assessment tool.
Thank you for your ongoing commitment and support for student clinical placements during these challenging times
Nurse and midwife researchers: Applications open for Future Leader Fellowship program

University of Melbourne and Melbourne Academic Centre for Health (MACH) are encouraging applications from fully qualified clinicians (including nurses and midwives) who are keen to bring Health Services Research (HSR) to bear on practical healthcare problems and take steps towards becoming a leader of innovative care.
The Future Leader Fellowship program will support a select cadre of established front-line clinical staff to address practical healthcare problems through HSR training and solutions. Without detriment to salary, each Fellow will be released from clinical duties for 0.2 FTE per week for 12 months, on a flexible basis, to upskill in HSR knowledge and work with (an) expert academic supervisor(s) to address a problem pertinent to their health service.
The program aims to bring clinicians with the best research-tractable ideas together with academic HSR experts to define the research needed to find an evidence-based solution to a practical healthcare problem. Deliverables at the end of the one-year fellowship could include an evidence-based solution to the identified problem, or more likely, a pilot study, collaborative application for research grant funding to address the problem, or a full-time problem-solving secondment such as those competitively offered by Safer Care Victoria. Fellows will continue to be paid in full by Western Health. On completion of the fellowship, the cohort will be supported by MACH to maintain regular interaction between themselves and the HSR experts with whom they have trained.
Formal part-time HSR training will be offered to the Fellows during the first six months of appointment in the form of registration for the University of Melbourne Master of Public Health (MPH) 6-month part-time elective in HSR. A scholarship will would provided to cover fees ($4,424 for those seeking assessment leading to 12.5 points towards the MPH; and $2,656 for unassessed work). The MPH elective in HSR will provide Fellows with formal training in HSR methods, coupled with time to begin refining the problem of interest for an HSR approach.
Eligibility
Eligible applicants must:
- Be a fully qualified Doctor, Nurse or Allied Health professional employed by a MACH-affiliated health service (vocational trainees are not eligible).
- Want to gain HSR expertise to share at the frontline.
- Have identified an important problem within their health service that could be addressed with a HSR solution.
- Show promise to become a leader in innovative care.
- Have written support from their manager to accompany their application (see below).
- Prior research experience is desirable.
Application procedure
Selection will be undertaken through an application and interview process led by the Director for MacHSR, Prof Harriet Hiscock. The highly competitive program will welcome up to 5 Fellows in the inaugural intake.
Pre-application enquiries may be sent to Lauren Wallis at University of Melbourne.
Applications should be sent by 9am Monday 21st March 2022 to lauren.wallis@unimelb.edu.au and must include:
- Full CV, including brief details of any research projects undertaken, the applicant’s role in the research, and how findings were disseminated (report for supervisors, abstract presentation at meeting, publication etc).
- A maximum two-page proposal outlining the practical problem of interest pertinent to the health service and how it might be addressed by HSR.
- A brief letter of support from the Health Service divisional/operational/professional manager responsible to senior management for the clinician’s unit confirming that the applicant is well placed to develop an interest in HSR, has the potential to become a future leader of innovative care, has in principle support for 0.2 FTE time-release from clinical duties if successful, and that the identified problem is important to address. An example letter template is available to view at www.machaustralia.org/MacHSR.
Interviews will be held in early May 2022 ahead of a mid July 2022 start.
Full details available at www.machaustralia.org/MacHSR
Benchmarking Best Care
The latest benchmark reports from the Health Roundtable that go up to September 2021 have recently been released, that show how our delivery of Best Care compares to other health services across Australasia.
In our continuing series looking at nursing and midwifery key performance indicators, this month we will look at how we perform in the area of pressure injuries. The following data looks at Western Health’s rate of Stage III, Stage IV, unspecified and unstageable pressure injuries, and suspected deep tissue injury.
Pressure Injuries:
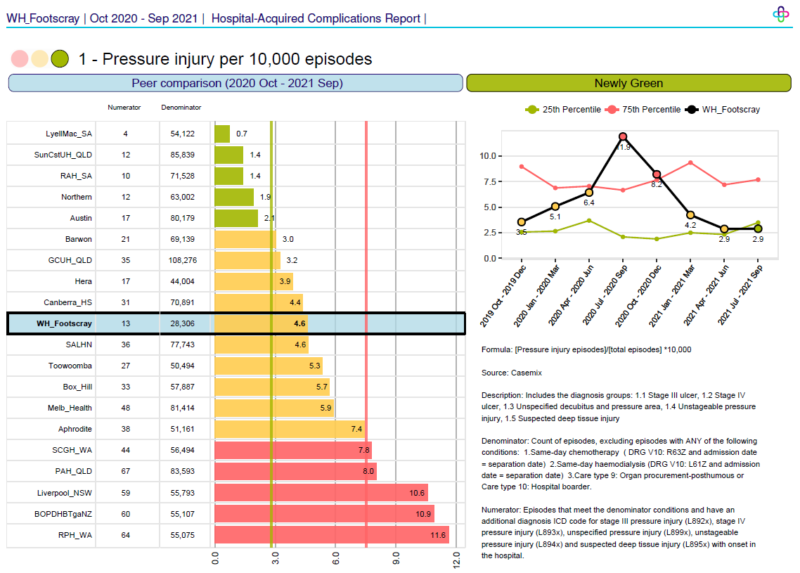
Footscray Hospital
There has been continued significant improvement in the Footscray Hospital rate of serious pressure injuries.
Just look at the drop over the past 15 months, and for the latest quarter we are green for the first time in a long time!!
Well done to all of our nurses at Footscray – what a remarkable achievement and your ongoing commitment to Best Care is really making a positive impact on our patient outcomes.
Let’s keep this going and sustain this great result!
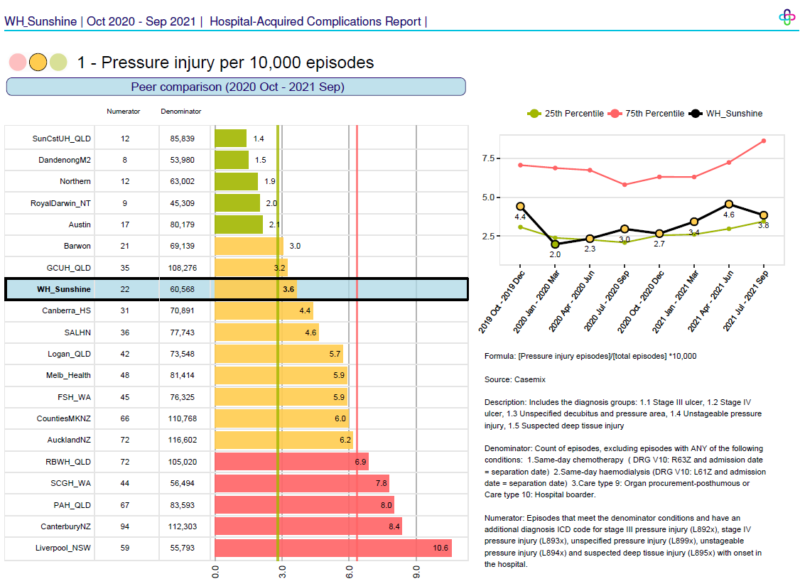
Sunshine Hospital
The rate of serious pressure injuries at Sunshine Hospital continues to be quite steady, but positively this is at the lower end of amber when compared to our peers.
The last quarter there has been a slight drop, and we are nudging green. This is really positive and means that we are nearly within the top 25th percentile of all Australasian comparable hospitals in terms of our rate of serious pressure injuries. Footscray Hospital’s hard work means that they are now in this elite group.
Keep up the great work Sunshine. We are so proud of our nurse’s commitment to continual improvement and providing our patients with Best Care.
Improving Cultural Safety
The Aboriginal Health Cultural Safety Plan 2019-21 had 4 objectives, whereby Western Health would:
- Improve communication and create a safe and welcoming environment.
- Have a culturally reflective workforce including our volunteers.
- Have evidence of Aboriginal health quality improvement, planning and research.
- Improve access to culturally appropriate services for Aboriginal and Torres Strait Islander people.
Despite many competing priorities and the distractions of COVID-19, Western Health’s Aboriginal Health Steering Committee and leadership team have shown commitment to implementing these objectives towards closing the health gap for Aboriginal and Torres Strait Islander people compared to non-Indigenous Australians. Examples of actions which have been fully implemented are:
- Provision of a room in the birthing suite that is welcoming and culturally sensitive for Aboriginal and Torres Strait Islander women.
- Flag Poles fly the Aboriginal and Torres Strait Islander flags at each hospital site.
- Develop Aboriginal communication and branding that is in place across Western Health and includes Aboriginal languages, cultural safety practices into relevant pages of the intranet and internet.
- Cultural Safety Audit Tool progressively utilised in clinical departments at all Western Health sites. Review of the physical environment and Reflections of how each unit works with Aboriginal and Torres Strait Islander patients and families.
- Reviewed the content of the Western Health Aboriginal Cultural Awareness online training
- Employees at Western Health participate in Aboriginal Cultural Awareness online training Programs
- Evaluate and refreshed the Western Health Aboriginal Employment Plan
- Review WH policies and procedures and update to reflect the NSQHS Version 2 Guidelines.
- Utilised opportunities to significantly expand and enhance Aboriginal Health Unit resources to enhance services. The team has significantly expanded, and recently appointed both a new Journey Walker position Ashleigh Vandenberg and a Research Fellow Dr Kunal Dhiman (jointly appointed with Deakin University).
- Implemented a dedicated Aboriginal community outpatients specialist service, expanding on the principles and factors that have led to the successful Galinjera midwifery program. This commenced in April 2021, informed by a research project carried out by Deakin University. “Barriers and Enablers to attending hospital appointments: Informing a new one-stop service for Aboriginal and Torres Strait Islander patients”.
- Development of a Western Health email signature incorporating an Acknowledgement to Country, Inclusion statement and Aboriginal and Torres Strait Islander flags.
- The Aboriginal Health Unit was renamed Wilim Berrbang (“Place of Connection” in Woi Wurrung language).
- The Western Health Foundation supported the purchase of 500 Welcome Packs for Aboriginal and Torres Strait Islander inpatients, containing a bathroom comfort kit, notebook and pen and information leaflets. Aboriginal and Torres Strait Islander bassinette blankets, knitted by volunteers, are given to families with a baby in the Special Care Nursery and patients at End of Life. All maternity families receive a knitted baby beanie in the Aboriginal or Torres Strait Islander flag colours.
- An Acknowledgement of Country is included in all meeting agenda templates and at the start of all education sessions held at Western Health.
The Aboriginal Health Cultural Safety Plan 2022- 2026
The Western Health Cultural Safety Plan 2022 – 2026 will integrate an Aboriginal Employment Plan. Recently extensive community, staff and stakeholder consultation was undertaken to inform Western Health’s Cultural Safety Plan 2022 – 2026. The plan is now in development, and it is proposed that it will be launched in NAIDOC Week (3rd – 10th July), which this year has the theme of ‘NAIDOC Week is Get Up! Stand Up! Show Up!’
Champions! You are invited to join new EMR network

Nurses and Midwives are invited to join the EMR Change Champion Network to help promote understanding of the EMR Phase 2.1 change.
It is a great opportunity to gain skills in change management (e.g. coaching, communication) and to help prepare your area and your fellow nurses/midwives for the Go-Live in April/May 2023.
The Change Champion Network will also prepare you to become an EMR Phase 2.1 Super User later in the year.
Training sessions for current nursing/midwifery Super Users will recommence soon, with an initial two Zoom classes scheduled for 28th April and 25th May 2022. Please book via WeLearn.
Please take a few minutes to answer the 6 question survey on EMR Phase 2.1. Your feedback will help the Digital Health team understand the current level of awareness of the EMR Phase 2.1 across the organisation so we can plan for the change. The survey closes at the end of March.
For more information on Super User training or joining the EMR Change Champion Network, visit the Digital Health information site.
New Changes to EMR Diet Orders

A number of changes to diet orders in the EMR will commence on 16 March 2022. Nurses and midwives should be aware of the following name changes, as well as new diet orders available in the EMR.
Diet Order Name Change for Food Allergy
- The diet order name will change to ‘xxxx FREE’ (i.e. Egg Free, Milk Free) for the most common food allergy causing a severe reaction such as anaphylaxis.
- The equivalent allergy order which is mapped from allergies and alerts in the EMR will be retained as ‘ALLERGY xxxx’. This allows the diet order to be used for patients without an allergy, but will ensure the most common allergies are separately identified in the allergy order.
- There is no change to the meals: the foods provided/allowed will be exactly the same for both the allergy and the diet.
- The naming of the allergies and diets follows the 2021 Australian Food Allergy Labeling Regulations and will now also include ‘Allergy Crustacea & Allergy Mollusc’ instead of ‘Allergy Shellfish’.
Name Changes
- ‘Pregnancy’ rather than ‘Maternity’ for the low listeria risk diet
- ‘Soft Dysphagia’ is now ‘Soft & Bite Size Dysphagia’ to reflect the International Dysphagia Diet Standardisation Initiative (IDDSI) definitions
New Diet Orders available in EMR
- ‘Eating Disorders Meal Plans 1-4’ to allow improved management of patients admitted with Eating Disorders
- ‘Cardiac PET HFVLC’ to assist the preparation of patients requiring a Cardiac PET
Emerging Evidence
The Western Health Library Service is a great source for locating the latest nursing and midwifery related evidence based practice and research.
New journal articles of interest:
- Australian women’s experiences of receiving maternity care during the COVID-19 pandemic: A cross-sectional national survey. Birth. 2022: March. Full Text Western Health Author
- An evaluation of interventions to improve outcomes for hospitalized patients in isolation: A systematic review. American Journal of Infection Control. 2022: February. PubMed Link. Request copy of article. Western Health Author
- Impact of Antimicrobial Stewardship Program on Antimicrobial Resistant and Prescribing in Nursing Home: A Systematic Review and Meta-analysis. Journal of Global Antimicrobial Resistance. 2022: February. Full Text
- Outcomes of Telehealth for Wound Care: A Scoping Review. Advances in Skin & Wound Care. 2022: February. Full Text
- Effectiveness of Interventions to Reduce Potentially Inappropriate Medication in Older Patients: A Systematic Review. Frontiers in Pharmacology. 2022: January. Full Text
- Patient-related risk factors for in-hospital functional decline in older adults: A systematic review and meta-analysis. Age and Ageing. 2022: February. Full Text
- Physician-to-Nurse Handover: A Systematic Review on the Effectiveness of Different Models. Journal of Patient Safety. 2022: January Full Text
- Nurses’ knowledge of heart failure self-care education: A systematic review. Nursing in Critical Care. 2022: February Full Text
New Nursing/Midwifery eBook Titles:
- Pocket guide for lactation management. 4th ed. Jones & Bartlett Learning, 2022.
This is an essential resource for new and experienced lactation care providers. Convenient and easy-to-use, it offers problem solving and counselling strategies for the wide-variety of situations commonly encountered by those working with child-bearing families. Topics include breastfeeding and public health, the Ten Steps to Successful Breastfeeding for hospitals and birth centres, normal breastfeeding, and addressing challenges from both the mother’s and baby’s perspective. - Emergency nurse practitioner core curriculum. Springer, 2021.
Written for Emergency Nurse Practitioners (ENP). Incorporating diversity and inclusion throughout, this resource contains all essential information needed for the provision of skilled care, including the history and development of ENP; fundamental clinical skills; management of medical emergencies, shock and trauma, and environmental emergencies; toxicology; emergency medical services and disaster preparedness; and the needs of special patient populations-all according to the most current evidence-based research and guidelines.
Off-site or home access to the library eBook titles, require free library membership. If you are not a member you can Join Online. For more information Click on our FAQ page.
Visit the library’s Intranet website, or ring the library to speak with a Librarian: 8395 8036 or 8345 6655. Working from home? Visit the Library Internet site.

