Applications close on Tuesday 5 April 2022 at 11:59 pm.
Western Health is a Platinum Affiliate of the ACN.
Employee Assistance Program: 1800 099 444
Nurse & Midwife Support: 1800 667 877
Nurse & Midwife Health Program:
03 9415 7551 or 1800 888 236
April 2022
5 Australian College of Nursing Scholarships and Grants applications close
13 Nursing & Midwifery Grand Round (2:30pm)
15 Good Friday Public Holiday
18 Easter Monday Public Holiday
25 ANZAC Day
26 Riskman 2 go live
27 Falls Improvement Plan launch (Grand Round)
30 Nursing Trailblazer Awards nominations close
Adjunct Professor Shane Crowe
Executive Director of Nursing & Midwifery
Phone: 8345 1463
Email: shane.crowe@wh.org.au
Allison Lamb
Acting Director of Nursing & Midwifery, Williamstown Hospital
Division: Aged Cancer and Continuing Care
Phone: 0421 950 501
Email: allison.lamb@wh.org.au
Professor Bodil Rasmussen
Chair of Nursing, Deakin University/Western Health
Phone: 8395 8163
Email: bodil.rasmussen@wh.org.au
Doug Mill
Director of Nursing & Midwifery
Divisions: Chronic & Complex Care, Drug Health
Phone: 8345 1916
Email: douglas.mill@wh.orh.au
Helen Sinnott
Director of Nursing & Midwifery, Sunshine
Divisions: Women’s & Children’s, Clinical Support & Specialist Clinics
Phone: 0435 962 716
Email: helen.sinnott@wh.org.au
Jo Mapes
Director of Nursing & Midwifery, Footscray Hospital
Division: Perioperative and Critical Care
Phone: 0423 302 337
Email: joanne.mapes@wh.org.au
Kate Renzenbrink
Director of Nursing & Midwifery Informatics (CNMIO)
Phone: 0425 772 324
Email: kate.renzenbrink@wh.org.au
Professor Linda Sweet
Chair of Midwifery, Deakin University/Western Health
Phone: 8395 1178
Email: linda.sweet@wh.org.au
Lisa Gatzonis
Director of Nursing & Midwifery Workforce
Phone: 9393 0127
Email: lisa.gatzonis@wh.org.au
Mandy Cullen
Acting Director of Nursing, Melton Health
Phone: 0413 867 065
Email: MandyCu@djhs.org.au
Nicole Davies
Director of Nursing & Midwifery, Sunbury Day Hospital
Division: Emergency, Medicine & Access, Western PHU
Phone: 9732 8630
Email: nicole.davies@wh.org.au
Rohan Vaughan
Director of Nursing, Bacchus March Hospital
Phone: 0434 365 769
Email: rohan.vaughan@wh.org.au
Sue Sweeney
Director of Midwifery Practice
Phone: 0466 801 447
Email: sue.sweeney@wh.org.au
Associate Professor Tony McGillion
Director of Nursing & Midwifery (Inspiring Innovation)
Phone: 0466 925 108
Email: tony.mcgillion@wh.org.au

This year Western Health has given out 107 full scholarships to nurses undertaking our ICU and ED post-graduate courses, and a further 42 additional scholarships to nurses undertaking post-graduate education in other specialties. This is our biggest ever investment in supporting our nurses to undertake post-graduate courses to gain specialty knowledge and skills, and it is terrific to see so many of our nurses furthering their own professional development.
Over this coming month we will officially launch our Falls Improvement Plan, which is the culmination of many months of work from a large number of dedicated people. This plan is a summary of planned actions and initiatives to ensure that we are doing everything that we possibly can to provide Best Care and reduce the number of falls and falls with injury. Whilst implementing best practice strategies and new pieces of equipment like the Proxi-mate system is exciting and important, I am really thrilled that the plan also includes supporting co-design methodology to engage multidisciplinary teams to generate strategies to ensure sustainable solutions. Working together to ensure that we really understand falls within a particular patient group and location, and then actively involving our clinicians so that they are part of the solution by identifying ideas on how to target local issues and improve outcomes is already leading to amazing results. It is wonderful to see the multidisciplinary teams working together, and many nurses taking the lead in this work and sharing their expertise to improve patient safety. I have high confidence that the improvements already achieved are just the beginning, and I encourage you all to get involved.
In maternity, this month Western Health will launch the Eve app to improve women’s involvement in their own care and improve the quality and timeliness of the best-practice, reliable information regarding pregnancy, birthing and early parenting. This is a huge leap forward in the provision of tailored health information in a contemporary way – but also will facilitate women getting information in their preferred language in the future. Additionally a 10 year retrospectively analysis of the clinical outcomes of women and their babies who requested Western Health homebirth program was recently published. Publicly funded homebirth programs are not common, so this is a really significant study as it shows that appropriate triaging, case selection, governance and clinical guidelines lead to homebirth being a safe option for women experiencing low-risk pregnancies. Well done to all our midwives involved in these important pieces of work.
Finally, we recently officially completed the Nursing & Midwifery Workforce Plan for 2019-21. This was an ambitious plan and pleasingly we were able to accomplish 25 actions and introduce many initiatives that have been pivotal to Western Health being able to maintain and enhance our nursing and midwifery workforce status despite the many challenges of the pandemic and our continuing rapid growth. The Plan had 3 priorities, and the outcomes included:
Attracting and retaining the best nurses and midwives
Empowering the provision of Best Care
Enhancing clinical and professional leadership
We are in the process of developing the Nursing and Midwifery Workforce Plan for 2022-26, which will be vital given the expected growth in our workforce due to new Footscray Hospital and other planned developments. There will be opportunities to influence this new plan, and I will keep you informed as it progresses.
Finally, the well-being of our nurses and midwives has been at the forefront of my mind throughout the COVID pandemic. Western Health has developed a Workforce Recovery Plan following the recent COVID surges, which outlines a synopsis of the strategies that the health service has in place to support the recovery of our people after some incredibly challenging years. A large proportion of the actions directly relate to supporting our nurses and midwives, and we will continue to adapt and evolve this plan to ensure that the needs of our workforce are met. If you feel that something is missing, please don’t hesitate to contact your Director of Nursing & Midwifery or myself – we welcome all ideas.
Shane Crowe
Executive Director, Nursing & Midwifery

Western Health established a Falls Taskforce to oversee the development and implementation of a Falls Improvement Plan, which is being officially launched on 27 April 2022.
To inform the plan, the Falls Taskforce has undertaken a gap analysis against best practice, and identified variations and opportunities. This included a detailed review of our own data trends, and those of our peers. There have been 4 busy sub-groups actively working under the Taskforce focusing on:
These sub-groups have developed recommendations following in-depth case reviews, and based on evidence based best practice which have informed the Falls Improvement Plan.
Additionally the Taskforce has sponsored the use of co-design methodology to engage multidisciplinary teams to generate strategies to ensure sustainable solutions. These strategies are supporting our teams to better understand their own falls data, enhancing accountability and responsiveness – and actively involve our clinicians so that they are part of the solution by identifying ideas on how to target local issues and improve outcomes.
All of the work planned by the Falls Taskforce for the next 2 years is summarised in Western Health’s Falls Improvement Plan, which is a dynamic, proactive and positive pathway forward. Pleasingly this Plan is already leading to active and productive initiatives that are making a huge difference by reducing our rate of falls and falls with injury. There has been some great improvements across our hospitals and wards, however we know that there is still a way to go. Our multidisciplinary teams are working in partnership with our patients to challenge traditional practices, implement improvements and embrace innovation. This is Best Care in action.
 The rates of homebirth in Australia remain low, at less than 0.3% of all births. Western Health has been running a publicly funded homebirth service for nearly 15 years (since 2009). A peer reviewed article has just been published in the Australian & New Zealand Journal of Obstetrics and Gynaecology (ANZJOG) retrospectively analysing the clinical outcome data over a 10 year period including neonatal outcomes of women who requested homebirth in Western Health’s program. The primary outcomes included: maternal outcomes (mortality, transfer to hospital, place and mode of birth, perineal status, type of third stage of labour, postpartum haemorrhage), and neonatal outcomes (mortality, Apgar score at five minutes, birthweight, breastfeeding initiation, significant morbidity, transfer to hospital).
The rates of homebirth in Australia remain low, at less than 0.3% of all births. Western Health has been running a publicly funded homebirth service for nearly 15 years (since 2009). A peer reviewed article has just been published in the Australian & New Zealand Journal of Obstetrics and Gynaecology (ANZJOG) retrospectively analysing the clinical outcome data over a 10 year period including neonatal outcomes of women who requested homebirth in Western Health’s program. The primary outcomes included: maternal outcomes (mortality, transfer to hospital, place and mode of birth, perineal status, type of third stage of labour, postpartum haemorrhage), and neonatal outcomes (mortality, Apgar score at five minutes, birthweight, breastfeeding initiation, significant morbidity, transfer to hospital).
Referrals for 827 women were reviewed, with 633 remaining eligible at 36 weeks gestation, and 473 (57%) birthing at home. Compared to women who did not, women who had a homebirth were significantly more likely to be multiparous, have a normal vaginal birth and an intact perineum, less likely to require suturing and less likely to have blood loss of more than 500 mL. Compared to infants not born at home, infants born at home were significantly less likely to require resuscitation, more likely to be of normal birthweight and exclusively receive breastmilk on discharge. There were no maternal deaths and one neonatal death of a baby born at home before the arrival of a midwife.
The outcomes have shown that for women accepted into Western Health’s publicly funded homebirth program suggest appropriate triaging, case selection, governance and clinical guidelines, appears to be a safe option for women experiencing low-risk pregnancies.
Well done to our Maternity Group Practice team for the excellent service you provide to women and the research team on this important article.
As an occupational group, healthcare workers are at increased risk of vaccine-preventable disease if not vaccinated. Additionally, if not vaccinated, healthcare workers may pose an increased risk of disease transmission to other workers and patients, particularly those who are vulnerable because of age, pregnancy, immunosuppression or chronic disease.
The introduction of mandatory vaccination of the influenza vaccination for Category A and Category B healthcare workers was recently announced by the Department of Health, and will be introduced this year. It will bring Victoria in line with other states and territories that have successfully introduced similar mandatory vaccination requirements.
Introducing mandatory vaccination of healthcare workers aims to:
Category A healthcare workers are those that have direct physical contact with patients, clients, deceased persons or body parts, blood, body substances, infectious material or surfaces or equipment that might contain these; or contact that might allow respiratory infections to be acquired or transmitted, for example workers with prolonged face-to-face contact with patients or clients or where their normal work is in a clinical area. Most Western Health nurses and midwives are in Category A.
Category B healthcare workers are those that work in patient areas who rarely have direct contact with blood or body substances. These employees may be exposed to infections spread by droplets, such as influenza.
Category A and B healthcare workers (current and newly commencing) are required to be vaccinated against seasonal influenza by 15 August 2022 and annually by 15 August each year following.
The preferred evidence of vaccination for Category A and B healthcare workers is an immunisation history statement from the Australian Immunisation Register (AIR).
More information will be shared as the Flu Vax program for 2022 launches.

The Nursing and Midwifery Health Program Victoria (NMHPV) did a lot of work in February 2022 with Western Health teams to provide support to our nurses and midwives.
NMHPV is conducting an important survey to check the health impact on nurses, midwives, and our students of working and living during the COVID-19 pandemic.
NMHPV is acutely aware nurses, midwives and our students have and continue to experience health impacts of working and living through the COVID-19 pandemic.
You are invited to take 10 minutes to complete this important ethics approved survey to assist NMHPV to understand the COVID-19 health impact on YOU.
Details and information about the survey, and the consent form are available at www.nmhp.org.au/survey, together with a link to the survey.

Medication safety and the provision of safe care at Western Health is vital to ensure positive outcomes for our patients.
A new poster to outline the nursing workflow on how to dispense and administer medication successfully has been developed and has recently been distributed. It outlines the 6 steps:
For APINCH medications: 2 authorised personnel to check at the bedside, verbal personal patient ID check (via the wristband), first authorised person administers the medication, the second person assists and witnesses. Both authorised persons co-sign the medication administration in EMR.
When all medication are administered, you can then sign the MAW.

In response to the COVID-19 pandemic, like other public health services, Western Health implemented surge models of care in response to unprecedented demand coupled with high numbers of furloughed staff and personal leave especially through the Delta and Omicron waves.
Western Health developed a Workforce Surge Plan in 2020, and had worked over an extended period of time through that year to prepare our staff for the potential impact of a surge. We proactively worked with our teams to educate them, up-skill and ready our teams in case this occurred. When the Department of Health released the COVID-19 acute care surge workforce delivery models there were strong synergies with the Western Health plan, and we adapted our plan to ensure alignment.
Melbourne’s West has been particularly hard hit by COVID in 2020 and 2021, and Western Health has been at the forefront with large COVID demand being managed by our teams. We have also supported large numbers of outbreaks in external locations including Residential Aged Care Facilities. Western Health has also had the added responsibilities of being a Local Public Health Unit and the COVID Vaccination Hub lead for the western metropolitan region.
Western Health has recognised that our clinical and non-clinical staff across all settings have been under extreme pressure, and proactive strategies have been put in place throughout the entire period to ensure that we care for our staff, so that they are retained as much as possible as we emerge from this difficult period. The wellbeing and safety of our staff is a core priority for Western Health, and this priority has been at the forefront of all our decisions since COVID emerged in 2019 and we commenced our own planning in late January 2020.
Whilst COVID related pressure on health services may reduce, there is always pressures in healthcare on the workforce and the return to ‘business as normal’ will bring with it new challenges.
Western Health is a rapidly growing heath service and proactive workforce management, maintaining a positive workplace culture and ensuring we are an employer of choice is central to us delivering high quality health services in an environment where our services are expected to almost double in size over the coming 6 years.
Western Health has been deliberate in our strategies and forward planning which have held us in good stead for our staff and services to emerge from COVID peak in a healthy position.
Western Health has developed a Workforce Recovery Plan which outlines a concise synopsis of the strategies that the health service has in place to support the recovery of our people. Western Health will continue to adapt and evolve our strategies, and where helpful will take on board ideas from the Department of Health and other services.

In February 2022 our incidence of Staph Aureus Bacteraemia (SABs) occurring at Western Health has increased. We need to nip this in the bud!
SABs are preventable, but incredibly serious with a 25% mortality rate. Western Health is usually a leader in our prevention of SABs, so we need to ensure that we get back to where we were.
During COVID-19 pandemic surge periods our audits have shown than in some cases staff have been wearing gloves for extended periods, wearing the same pairs of gloves between patients and decreasing the frequency of hand hygiene.
It is important that we all keep ourselves safe, however the practice changes that have been adopted by some do not align to our PPE guidelines or Infection Prevention procedures and are inadvertently increasing risk to our patients. None of us want that to occur.
SABs are prevented by simple, good infection prevention practice. There is an improvement event occurring during January to focus on the key factors that prevent SABs:
Thanks to everyone that is reflecting on their own practice. Together we can turn this around and ensure that our patients are safe.
National Closing the Gap Day occurred on Thursday 17 March, and acknowledges the ongoing strength and resilience of Aboriginal and Torres Strait Islander people in sustaining the world’s oldest living cultures.
Closing the Gap is underpinned by the belief that when Aboriginal and Torres Strait Islander people have a genuine say in the design and delivery of policies, programs and services that affect them, better life outcomes are achieved. It also recognises that structural change in the way governments and health services work with Aboriginal and Torres Strait Islander people is needed to close the gap.
Western Health is an official signatory to the National Close the gap Statement of Intent. Along with Wilim Berrbang, our Aboriginal Health Unit, Western Health continues to work towards equality of health access and outcomes and ensuring an equitable voice for Aboriginal people. Examples of this in action are:
Western Health is committed to delivering culturally safe health care to our Aboriginal and Torres Strait Islander patients and families. Watch out for the launch of our 2022-2025 Cultural Safety Plan Plan which outlines Western Health’s commitment to building on the efforts and progress we have made through the successful implementation of our past Aboriginal Health Cultural Safety Plans and Aboriginal Employment Plans. This Plan also articulates how we can attract Aboriginal and Torres Strait Islander candidates to our growing health service and support these employees to thrive in their roles.
On Wednesday 16 March 2022 World Delirium Day was held, as an annual day of delirium recognition, education, and prevention through community engagement. Did you know that evidence shows that delirium effects 25% of medical patients, 50% of surgical patients and 75% of ICU patients! There are no medications approved for the treatment of delirium. Clinicians treat delirium by identifying and treating the underlying causes.
Here are some actions you can take to stop delirium:
You can help prevent delirium by:
Western Health recognised this World Delirium Day with a information table staffed by our resident experts, including our Clinical Nurse Consultant for Delirium and Cogitative Health Sharon Collard.
The latest benchmark reports from the Health Roundtable that go up to September 2021 have recently been released, that show how our delivery of Best Care compares to other health services across Australasia.
In our continuing series looking at nursing and midwifery key performance indicators, following the recent National World Delirium Day this month we will look at how we perform in the area of delirium.
Delirium:
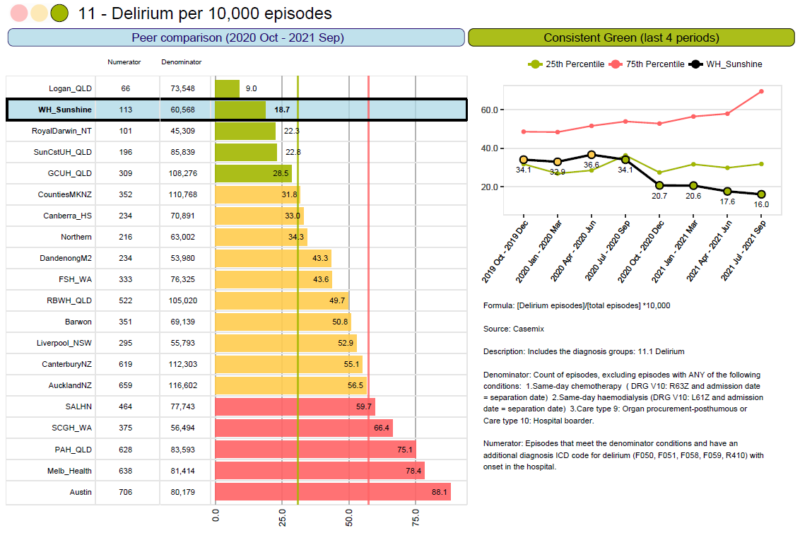
Sunshine Hospital
The rates of delirium at Sunshine Hospital is in the green when compared to our peers, and keeping consistently low and dropping. This is a fantastic result.
Well done to our Sunshine Hospital teams.
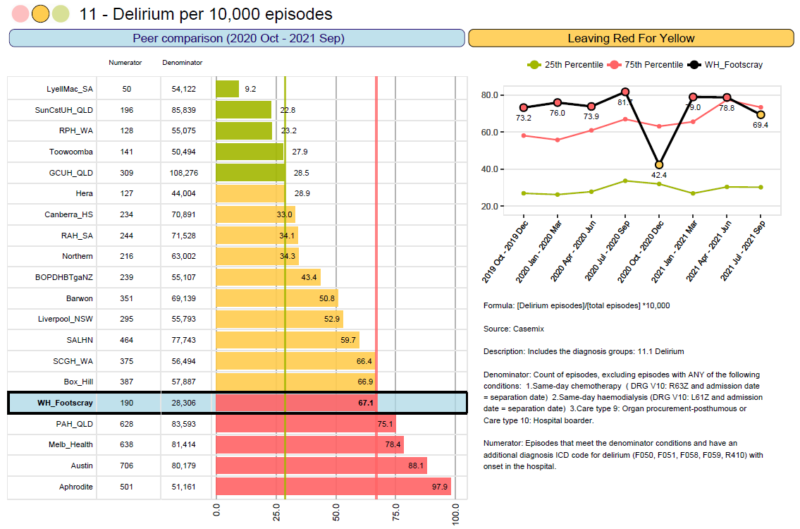
Footscray Hospital
Rates of delirium at Footscray Hospital remain higher, however have dropped slightly over the past quarter going into amber for the first time in 9 months.
Footscray Hospital has a lot of surgical activity, and 50% of surgical patients can be effected by delirium unless we put active steps in place to prevent it wherever possible. We can do this through frequent reorientation, early and recurrent mobilisation, pain management, adequate nutrition and hydration, reducing sensory impairments, and ensuring proper sleep patterns. If you need any support, please contact Sharon Collard (CNC Delirium and Cognitive Health).

Rapid Assessment Discharge Unit (RADU) has started operating from the 7 March at Sunshine Hospital in 2G. RADU is a 24 bed inpatient unit for medical patients with an expected length of stay less than 48 hours. The aim of the unit is to improve patient outcomes with a shorter length of stay and excellent assessment and care provided by a group of specialist clinicians in a shorter time span. By focusing on this patient group, the RADU aims to assist in improving access and flow of patients through Western Health.
RADU is aiming to get their patients primarily via ED, but may also get admissions from HITH, community programmes or clinics as well. RADU admissions aim to meet ED NEAT KPI of<4 hours.
Once admitted to RADU, all patients are expected to get nursing, medical and allied health assessment within 4 hours of admission and patients will be informed of their discharge time and care plan. The RADU team consists of a medical team lead by 2 medical consultants and an aged care consultant, nursing team led by NUM and ANUMs and an allied health team on extended hours 7 days/week. Once fully recruited pharmacy will have an extended coverage during weekdays and weekends as well.
RADU will be a great addition to Western Health in achieving more positive patient outcomes and a better flow of patients through Sunshine Hospital once operating to its full capacity.

The impact of COVID-19 in the Australian community has resulted in a significant decrease in the number of blood donations over the past 2 years with resulting supply challenges. Supply has been further challenged with the recent flooding in Queensland and northern New South Wales decreasing the number of donations.
For some blood products and blood groups Red Cross Lifeblood Victoria have implemented inventory restrictions. This requires the blood bank scientists to place MO patient orders for that specific product. These orders are then triaged and approved by a Lifeblood Transfusion Medicine Specialist.
Judicious attention to patient blood management for all transfusion decisions for RBC, platelets and frozen blood products (i.e. FFP and cryoprecipitate) and meticulous attention to the transport and storage of blood products to negate avoidable wastage is always important, but it is critical in times of supply shortages such as we are currently experiencing.
For more information on how you can make a difference please read this Blood Product Shortage during COVID QRG.

Nominations for the 2022 round of the prestigious Health Minister’s Award for Nursing Trailblazers are now open.
The award is the first of its kind in Australia, and acknowledges the vital role nurses play in transforming our country’s health and aged care systems.
Since its launch in 2019, the award has provided a national platform to profile the achievements of innovative nurse leaders.
Among others, Trailblazer Winners and Finalists have been recognised for contributing to evidence-based nursing care for stroke patients, integrating specialist palliative care into residential aged care facilities and using nurse-led models to transform and improve the quality of care for cancer patients.
Wouldn’t it be nice if a Western Health nurse was recognised via this award?
If you are a driven nurse leader who uses evidence-based processes to transform our health and aged care systems we encourage you to showcase your accomplishments by nominating yourself for the 2022 Health Minister’s Award for Nursing Trailblazers.
You can also nominate a nursing colleague who you think deserves to be acknowledged for their achievements.
Nominations close 30 April 2022.
If you have any queries please feel free to get in touch by contacting the Australian College of Nursing via engagement@acn.edu.au.
What is Aboriginal Cultural Awareness?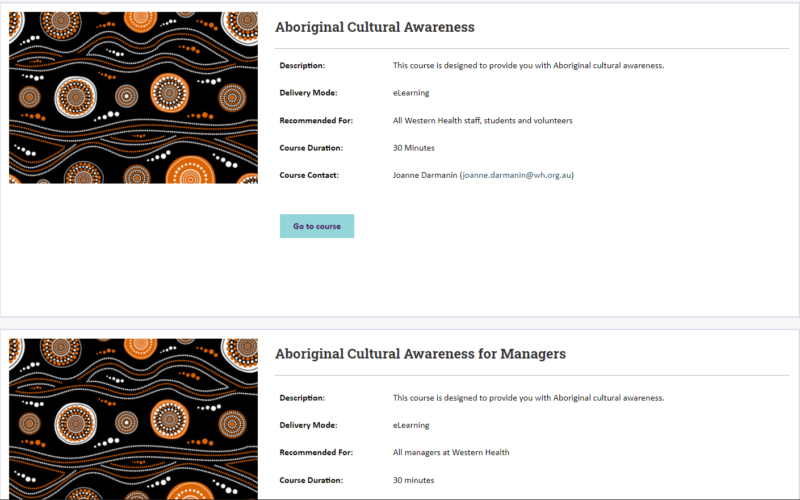
Cultural awareness is a basic understanding of Aboriginal and Torres Strait Islander histories, peoples and cultures. It is generally accepted as a necessary first step and a foundation for development and change.
What is cultural safety?
Cultural safety is defined by the patient’s experience – the individual’s experience of the care they are given, and their ability to access services and to raise concerns, not by the health professional. The presence or absence of cultural safety is determined by the experience of the recipient of care and not by the staff member.
The essential features of cultural safety are:
Cultural safety does not propose that people become experts on other cultures, it places an emphasis on understanding that there are cultural differences.
Our goal is for Western Health to have a culturally reflective workforce where we can reflect on our own cultural norms and beliefs, and how these impact on the way we provide care to others from a different cultural and spiritual background.
Completing the Aboriginal Cultural Awareness Training on We Learn is a great first step in the ongoing journey of reconciliation, is a foundation for cultural awareness and will assist in ensuring cultural safety for our Aboriginal and Torres Strait Islander patients and families.
Have you completed the Aboriginal Cultural Awareness Training on We Learn?

Applications for the Australian College of Nursing (ACN) Scholarships, Grants and Awards are now open.
If you are looking for financial assistance to help you pursue your health care education goals these are a great option for nurses.
ACN administers a range of Australian Government Department of Health scholarships for undergraduate and postgraduate aged care, nursing and midwifery courses as well as scholarships for Aboriginal and Torres Strait Islander students studying entry-level health courses. Please click on this link to find out more, search the range of scholarships to see how ACN can support you and apply. There are different opportunities for fellow, members and non-members.
The ACN Foundation also offer grants and awards to support nurses to complete continuing professional development as well as postgraduate study and research. You can read more about these exciting opportunities at the bottom of this page.
Since the Royal Commission into Victoria’s Mental Health System delivered its final report on 3 February 2021, major changes have taken place to reform mental health delivery and lay the foundations for further significant changes. This includes the development of a new Mental Health and Wellbeing Act, the start of the recruitment for the Interim Regional Boards, and the development and release of the Mental Health and Wellbeing Workforce Strategy.
On 21 March 2022 our Chief Executive Russell Harrison provided an update that on the implementation of mental health service delivery reforms across north and west metropolitan Melbourne. These reforms are part of the proposal from the Royal Commission into Victoria’s Mental Health System to provide a more accessible, responsive and well-resourced mental health service system for consumers and communities in these catchments.
The update went into detail regarding the transition of mental health services in north and west Melbourne and outlines key changes for the health services involved including Western Health, Northern Health, Mercy Health, Austin Health, Royal Melbourne Hospital, Royal Children’s Hospital and Orygen.
The key change for our health service is that Mid West Area Mental Health Services will separate from the Royal Melbourne Hospital’s NorthWestern Mental Health and Mercy Mental Health services for Maribyrnong will separate and both will come together to be operated by Western Health by mid 2023. We welcome this change and look forward to these staff joining Western Health next year.
Once our colleagues in the north have transitioned services we will commence working with North West and Mercy Mental Health on the detailed plan to support the transition of staff and services to Western Health and we will share more specifics in the near future. But it is important to note there will be no job losses in any of the services and for many impacted staff their employment will not change.

On 4 April our maternity team at Western Health are launching the Eve App, which is a mobile app designed to enable pregnant women and new mothers to have access to information and assistance to enhance their pregnancy and early parenting experience.
The implementation of the Eve App aims to improve women’s involvement in their own care and improve the quality and timeliness of the information they were seeking regarding pregnancy, birthing and early parenting.
When women book in to have their baby at Western Health, they will receive a SMS inviting them to download the application. This will be linked to their specific booking and their own medical record and will have bank-level encryption to ensure privacy is maintained. Women will receive weekly updates about how their body is changing and baby is growing and have new articles that are relevant to their stage of pregnancy/parenting. They can also search for specific articles or topics that they are interested in.
The Eve app has practical content such including:
The educational content is initially available in English, however Western Health will be working collaboratively with the company and other health services to make resources available in other languages in the future.

Nurses and Midwives working in the Emergency Department can take a first look inside the new EMR ED system, which is called FirstNet.
FirstNet will be implemented in the Footscray, Williamstown and Sunshine ED’s in the EMR Phase 2.1 Go-Live which is planned for April – May 2023.
FirstNet will replace the current ED system EDIS, as well as many paper forms, and will streamline and integrate the documentation from ED to our inpatient spaces.
Elle and Alan from the Emergency, Medicine and Access EMR Phase 2 Project Team feature in a short video which provides a glimpse inside the new system as well as a look at the functionality it will provide.
You can view the video here.
For further information please contact Kyrin Sandles, Project Manager, EMR Phase 2 Emergency, Medicine and Access – Kyrin.Sandles@wh.org.au.

GIANT STEPS 2022, Victoria’s best (and only) healthcare quality and safety conference will take place on Thursday 26 and Friday 27 May. Bringing together all those interested in finding a better, safer way to deliver healthcare in Victoria.
The start of 2022 has not been easy on our healthcare workers. In recognition of their efforts, Safer Care Victoria are providing a 30 per cent discount to attend an unforgettable two-day quality and safety conference. In person tickets are now only $490, and virtual tickets $320.
The program includes a great range of interesting speakers, featuring:
There is also plenty of local and national talent sharing their experiences and stories.
Book your ticket now!
And not to worry, as life can be unpredictable, so please note that Safer Care Victoria will happily provide full refunds if COVID-19 prevents paid ticket holders from attending.

A reminder that the new version of Riskman will be launched on 26 April 2022 on most Western Health sites. Bacchus Marsh/Melton will move to the new system closer to the end of June 2022.
The upgraded Riskman will be more user friendly and intuitive than our existing register.
Changes you will notice in the upgraded Riskman are as follows:
One hour Zoom training sessions are available to support staff to understand the updated layout of the new Riskman during double staff times of 1.30pm to 2.30pm on Mondays, Tuesdays, Wednesdays, Thursday’s and Fridays (except on public holidays). Find out more about these sessions by clicking here
There is also a WeLearn Training video video that introduces the upgraded system and demonstrates the key changes.
Further information can be found on the Best Care Microsite

An uplift to the Pain Management View Band and iView Documentation of Analgesic Infusions in the EMR will take place on Wednesday 6th April.
The uplift will further streamline the documentation of PCA Analgesic Infusion with a Zero (0) rate in the Pain Management View Band. This will allow
These sections are where you will document or review:
To complement this rollout, a new WeLearn package is now available for ‘Completing an Analgesic Infusion – PCA with Zero ‘0’ Rate.
A Quick Reference Guide has also been created to assist with this change.
For further education on this change, please contact the Acute Pain Management Service (APMS) team – Davina.Taylor@wh.org.au.
The Western Health Library Service is a great source for locating the latest nursing and midwifery related evidence based practice and research. The links below work best with Microsoft Edge or Chrome.
Articles of interest:
New Nursing/Midwifery eBook Titles:
Training:
Custom Library Training Offers:
Our team of Medical Librarians are trained to assist you with many types of research support, from beginner journal article searching help, to advanced searching/research skills. We offer custom, targeted training sessions – on request through Zoom. Please reach out to request a training session specifically for your requirements. We are here to help.
Off-site or home access to the library eBook titles, require free library membership. If you are not a member you can Join Online. For more information Click on our FAQ page.
Please Contact us for Library Locations and Opening Hours.